Transforming cardiology outcomes with digital health and eHealth innovations
- Digital health and innovation is a rapidly growing field in healthcare.
- eHealth is representative of the health care data and records that cannot be stored within mobile health applications.
- These technologies enhance the overall quality of life for patients and care experiences, lower healthcare costs, and empower patients and providers.
- Healthcare professionals and patients both are managing cardiovascular diseases like hypertension, atrial fibrillation, coronary artery disease, and heart failure in a novel manner because of digital health, particularly telemedicine, and mHealth.
What is digital health?
Digital health is defined as the knowledge and practice of adopting any aspects of digital techniques that help in improving health, from inception to operation1.
What is eHealth?
The utilization of information and communications technologies that are both cost-effective and safe has become essential in promoting health and supporting health-related fields. This includes services in health care, health surveillance, health literature, health education, knowledge, and research1.
The ten “e’s” that characterize eHealth2 help in maintaining a balance of information and communication between healthcare practitioners and patients/users are listed in Figure 1.
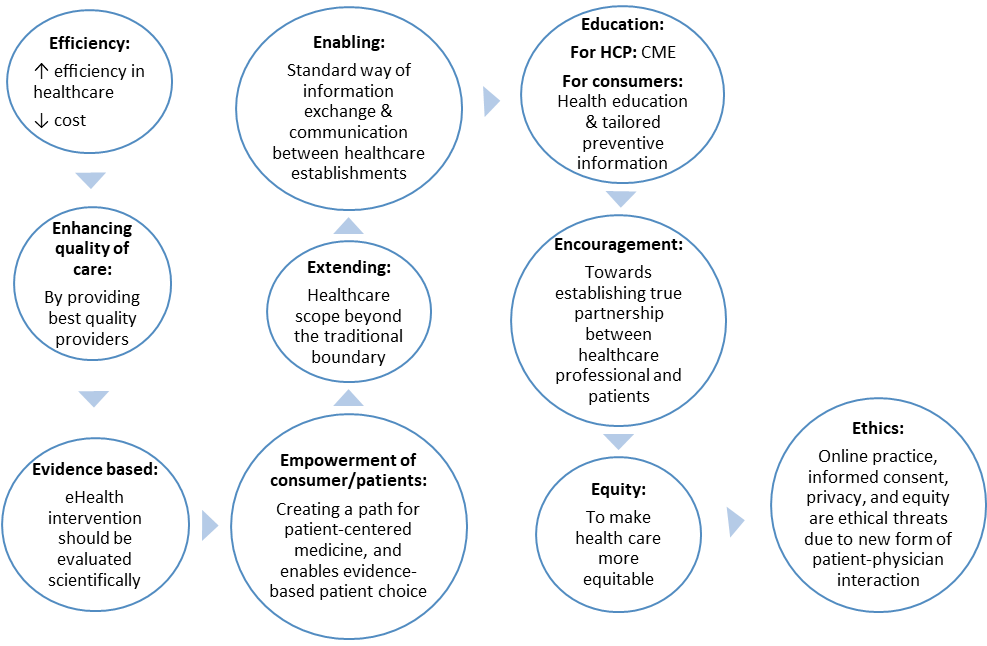
Figure 1: Characteristics of eHealth2
Digital health in cardiology
Incidence of CVD is rising globally3, and they are the leading cause of death worldwide, therefore, require advancing technology4 to win the battle against the growing burden of CVD. Telemedicine has been extensively used in cardiology. The two most popular techniques are:
Telemonitoring: Various innovations in digital health are impactful in CVD; the most popular is blood pressure telemonitoring (BPT). It helps in controlling blood pressure as individuals regularly monitor their BP and therefore are more adherent to medication5 using such tools. For instance, a meta-analysis of studies on hypertension showed that in addition to traditional therapy, regular BPT home practice with a follow-up period of at least six months corresponds to a significant decline in both office and 24-h ambulatory BP in 7037 individuals6.
Tele-visit: This is an important technology for video consultation between clinicians and patients to avoid follow-up visits. The impact of this technique has been evaluated in a study where monthly teleconsultation through videoconferencing was implemented with at least one face-to-face clinical visit for acute ST-elevation myocardial infarction patients. The patients were found more adherent to medication and followed a healthy lifestyle after 3 months7.
Latest digital health innovations for improved patient outcomes in cardiology
Techniques have been transforming the healthcare sector over the past ten years through numerous advancements. A recent systematic review and meta-analysis highlighted the role of digital health interventions in reducing CVD risk (Relative Risk 0.61, 95% CI, 0.46–0.80) along with weight (−3.35 lbs, (95% CI, −6.08 lbs, −1.01 lbs) and body mass index −0.59 kg/m2, (95% CI, −1.15 kg/m2, −0.03 kg/m2) management 8.
Recent technologies in digital health, such as wearables, sensors, eHealth, mHealth, telemedicine, and artificial intelligence (AI), have offered possibilities to enhance healthcare access and delivery9. Some of the innovations in digital health for the prevention and management of CVD are as follows:
a) Wearables and sensors
One of the independent risk factors for CVD is non-dipping heart rate (HR); however, it is neglected during CV risk assessment. This phenomenon of dipping HR is usually encountered with adverse CV prognosis. Smartwatches and fitness trackers are available with various technologies and sensors to track health parameters; however, photoplethysmography (PPG) is considered best. It detects changes in blood volume in the subcutaneous tissue based on the interaction of light with blood in the tissue 10.
Various clinical studies have reported the accuracy of consumer-grade wrist-worn devices for monitoring heart rate (HR) during a free-living activity like sleep, rest, post-exercise, and daily routine activity11-13. The results demonstrate the faithfulness of wrist-worn devices in replicating a circadian HR rhythm during free-living and detecting HR during routine activities and night-time. These devices could be used for CV risk assessment in hypertension. They are cost-effective and can curb long-term healthcare expenses in high-risk patients during primary care for hypertension.
b) Telemedicine/Telehealth
- Blood pressure telemonitoring through “cuffless” devices based on wrist tonometry or finger photoplethysmography are gaining popularity14 as they overcome the discomfort and inconvenience of using cuff-based measurement.
Telehealth specifically, video-visit and remote patient monitoring15,16 are the new digital technologies that focus on unique aspects of care delivered by the healthcare provider for the advancement of patient-clinician communication.
- Patients in the video-visit group are reported to be at a lower risk of heart failure and readmission at 6 months as compared to the patients who visited in person17.
- An implantable pulmonary artery sensor is another advancement in digital health. It describes the benefits of remote patient monitoring (RPM). In RPM, patients obtain physiological data from the home location5 which is reviewed by clinician/healthcare on a routine basis15. This device monitors the ambulatory pressure in heart failure patients and the data is used by clinicians to titrate the medication as well as lifestyle modifications15. The effect of the implantable pulmonary artery sensor could be seen in future pressure readings. It also benefitted patient participation and improved outcomes18.
- A pedometer or home-based teleintervention can increase the physical activity in those patients who do not attend any cardiac rehabilitation (CR) program in hospitals19. Physical activity is core to a healthy lifestyle, and it also reduces the risk of cardiovascular diseases and other chronic diseases. It was observed that pedometer-based telephone coaching increases the physical activity in both those who attend CR programs as well as who don’t attend the same. The cost-effectiveness and robustness of this technique is responsible to enhance physical activity and longevity in cardiac patients especially in participants in rural areas who did not attend CR19.
c) mHealth
- mHealth applications for medication adherence: Various mHealth apps are in use to enhance adherence to medications for dyslipidemia, CVD, heart failure, etc. These applications can act as reminders and record medication-taking activity for later evaluation of adherence. Apps like “My A:care” are based on behavioral models to motivate and guide patients to build medication adherence behavior for life. For more on mobile health apps, please read our article Mobile apps for enhancing adherence to chronic diseases.
- WhatsApp in mHealth4: Use of WhatsApp and a client-server architecture for the exchange of hemodynamic images in cardiology. Five dynamic photos were used in a clinical setting to evaluate the WhatsApp system under strict guidelines. Five interventional radiology professionals examined the system, giving it excellent marks for use, utility, and speed and average marks for picture quality and technology.
- mHealth intervention for dietary behavior4: mHealth programs via text messaging have been shown to improve lifestyle and dietary behavior in CVD. Six months of intervention with this approach has shown effective results in some studies. The mHealth studies are less in low-middle income countries. Further studies can be targeted to improve disease behavior in such regions.
- Smartphone-based AI in cardiology4: AI is a potential technology in cardiology that offers a variety of utilities, such as clinical risk estimation, digital image analysis: collecting data, and quality control. Despite its potential, further studies are required for its frequent use in cardiology.
d) Conversational agents or Avatars
- Another interesting innovation in cardiology is “Conversational agents/virtual coach/Avatars”. A recent report described that virtual agents/avatars were able to accomplish diet management, weight, physical activity, and to some extent hypertension. However, the data and clinical trials for the same are few, therefore further studies would be required to support the effectiveness and efficiency of virtual coaches20.
Further research is required to improve our knowledge of the potential benefits of emerging digital tools for CVD management and prevention, such as wearable gadgets and social networks, as well as to scale up and integrate these tools into daily practice.
To know more about use of technology to enhance medication adherence please read: Technological advancements and innovations to improve medication adherence. and Looking into the Crystal-ball: Advances in technology for improving adherence.
Digital health strategy in cardiology
To make digital health a standard of care, both healthcare professionals and users require comprehensive knowledge to utilize and implement digital health interventions. To achieve this goal we must first build the foundation by joining the following priorities:
- Patient-centered co-design
The “Theory of Reasoned Action,” which describes the connection between human attitudes and behaviors, is the basis for technology acceptance models, and it states that the key factors that determine the adoption of technology in patient care are its perceived usefulness and ease of use, which remains rooted within the core principles of adoption15:
- Functionality & operational efficiency at the individual level
- The flow of digital information between the patient, caregiver, and clinician
- Post-implementation strategies based on continuous testing and user feedback
Co-design was evaluated upfront before RPM implementation in the eHealth platform for self-management of CVD and Cardiac rehabilitation15. While co-design focuses on overcoming major adoption barriers for new technologies, it may also be used to develop a monitoring strategy to determine which technology functions best and in whom15.
- Remote patient monitoring program (RPM)
Remote patient monitoring is a program used to generate patient data outside the clinical setting that can be reviewed by a clinician regularly15. This program helps in patient participation and self-management.
- Electronic phenotyping
Using a simplistic logic-based (yes/no) method and a lack of generalizability makes current clinical design support (CDS) static. However, current advancements in data analytics such as electronic phenotyping can find patterns in the data that may be utilized to create CDS systems. The framework of electronic phenotyping classifies structured digital information into vectors and uses them to characterize patients using a set of encoded representations.
Digital health devices enable continuous data collection and processing, which leads to the creation of larger and more detailed data sets and thus an electronic phenotype of a particular disease and its severity15. It can be later used to rule out the stages or severity of the disease to help administer the type of digital health technology and monitoring strategies15.
“Innovation is taking two things that already exist and putting them together in a new way.”- Tom Freston
References
1. Organization WH. Global strategy on digital health 2020-2025. Geneva. 2021.
2. Eysenbach G. What is e-health? J Med Internet Res. Apr-Jun 2001;3(2):E20. doi:10.2196/jmir.3.2.e20
3. Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J Am Coll Cardiol. Dec 20 2022;80(25):2361-2371. doi:10.1016/j.jacc.2022.11.005
4. Islam SMS, Maddison R. Digital health approaches for cardiovascular diseases prevention and management: lessons from preliminary studies. Mhealth. 2021;7:41. doi:10.21037/mHealth-2020-6
5. Omboni S. Connected Health in Hypertension Management. Front Cardiovasc Med. 2019;6:76. doi:10.3389/fcvm.2019.00076
6. Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens. Mar 2013;31(3):455-67; discussion 467-8. doi:10.1097/HJH.0b013e32835ca8dd
7. Kamel H, Hafez MS, Bastawy I. Telemedicine Improves the Short-Term Medical Care of Acute ST-Segment Elevation Myocardial Infarction After Primary Percutaneous Coronary Intervention. Front Cardiovasc Med. 2021;8:693731. doi:10.3389/fcvm.2021.693731
8. Widmer RJ, Collins NM, Collins CS, West CP, Lerman LO, Lerman A. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc. Apr 2015;90(4):469-80. doi:10.1016/j.mayocp.2014.12.026
9. Murray E, Hekler EB, Andersson G, et al. Evaluating Digital Health Interventions: Key Questions and Approaches. Am J Prev Med. Nov 2016;51(5):843-851. doi:10.1016/j.amepre.2016.06.008
10. Baka T, Simko F. Monitoring Non-dipping Heart Rate by Consumer-Grade Wrist-Worn Devices: An Avenue for Cardiovascular Risk Assessment in Hypertension. Front Cardiovasc Med. 2021;8:711417. doi:10.3389/fcvm.2021.711417
11. Gillinov S, Etiwy M, Wang R, et al. Variable Accuracy of Wearable Heart Rate Monitors during Aerobic Exercise. Med Sci Sports Exerc. Aug 2017;49(8):1697-1703. doi:10.1249/MSS.0000000000001284
12. Reddy RK, Pooni R, Zaharieva DP, et al. Accuracy of Wrist-Worn Activity Monitors During Common Daily Physical Activities and Types of Structured Exercise: Evaluation Study. JMIR Mhealth Uhealth. Dec 10 2018;6(12):e10338. doi:10.2196/10338
13. Wang R, Blackburn G, Desai M, et al. Accuracy of Wrist-Worn Heart Rate Monitors. JAMA Cardiol. Jan 1 2017;2(1):104-106. doi:10.1001/jamacardio.2016.3340
14. Bard DM, Joseph JI, van Helmond N. Cuff-Less Methods for Blood Pressure Telemonitoring. Front Cardiovasc Med. 2019;6:40. doi:10.3389/fcvm.2019.00040
15. Bhavnani SP. Digital Health: Opportunities and Challenges to Develop the Next-Generation Technology-Enabled Models of Cardiovascular Care. Methodist Debakey Cardiovasc J. Oct-Dec 2020;16(4):296-303. doi:10.14797/mdcj-16-4-296
16. Joseph P. Lyons KWaAM. The Evolution of Elderly Telehealth and Health Informatics. In: Edoh KSaT, ed. Recent Advances in Digital System Diagnosis and Management of Healthcare. 2019.
17. Comín-Colet J, Enjuanes C, Verdú-Rotellar JM, et al. Impact on clinical events and healthcare costs of adding telemedicine to multidisciplinary disease management programmes for heart failure: Results of a randomized controlled trial. J Telemed Telecare. 2016;22(5):282-295. doi:10.1177/1357633X15600583
18. Krishnaswami A, Beavers C, Dorsch MP, et al. Gerotechnology for Older Adults With Cardiovascular Diseases: JACC State-of-the-Art Review. J Am Coll Cardiol. Dec 1 2020;76(22):2650-2670. doi:10.1016/j.jacc.2020.09.606
19. Sangster J, Church J, Haas M, Furber S, Bauman A. A comparison of the cost-effectiveness of two pedometer-based telephone coaching programs for people with cardiac disease. Heart Lung Circ. May 2015;24(5):471-9. doi:10.1016/j.hlc.2015.01.008
20. Lyzwinski LN, Elgendi M, Menon C. Conversational Agents and Avatars for Cardiometabolic Risk Factors and Lifestyle-Related Behaviors: Scoping Review. JMIR Mhealth Uhealth. May 25 2023;11:e39649. doi:10.2196/39649
