Unravelling the path on how to improve medication adherence
- About half of individuals with chronic conditions fail to adhere to their prescribed medication regimens. This lack of adherence not only elevates the risk of health complications and mortality but also leads to significant financial burdens annually. 1
- Non-adherence, intentional or unintentional, needs understanding to create effective adherence strategies.2
- Brief, validated self-report measures in clinical settings can both predict patient outcomes and provide actionable insights into medication nonadherence.3
- Research shows that while poor medication adherence is associated with reduced therapeutic success, lower quality of life, and higher treatment costs, good adherence is linked to lower mortality rates in clinical studies.4
- Poor medication adherence is influenced by various factors, including patient literacy, physician communication, and systemic healthcare limitations.1
Medication adherence is a multi-faceted concept extending beyond taking prescribed drugs to include numerous health-related behaviors. Recognized by the World Health Organization (WHO), this concept encompasses an array of interventions critical for chronic disease management, highlighting the necessity for active patient involvement in treatment processes. Behaviors like seeking medical attention, prescription filling, lifestyle changes, and correct medication usage form the crux of adherence.1
The relationship between the patient and healthcare provider forms the cornerstone of effective adherence. Open discussions about treatment options, adherence, and planned follow-ups characterize successful treatment partnerships. Precise adherence to prescribed guidelines is critical, with non-adherence causing significant health consequences.5
Understanding the root causes of poor medication adherence is crucial for designing effective interventions. According to the WHO, these causes generally fall into five categories: socioeconomic, therapy-related, patient-related, condition-related, and healthcare system/team-related factors. By identifying whether the nonadherence is primary (starting treatment) or secondary (following the prescribed regimen), and pinpointing the contributing factors, personalized interventions can be developed to improve each patient’s medication compliance.6
Understanding the types of non-adherence
Recognizing the intricate factors that affect medication adherence for chronic conditions is crucial for avoiding patient blame and identifying effective solutions.1
Non-adherence can be classified into two types: intentional and unintentional.
- Intentional non-adherence occurs when a patient chooses to deviate from their prescribed regimen consciously. Their beliefs, preferences, and perceptions of the treatment, as well as their motivation to initiate and continue with it, all influence their behavior. Intentional non-adherence can be influenced by factors such as perceived side effects, misunderstandings about instructions, or a belief that the medication is unnecessary. 2
- Unintentional non-adherence, on the other hand, occurs when patients inadvertently fail to follow the prescribed treatment. This can be due to a variety of factors such as forgetfulness, misinterpretation of instructions, financial constraints, or external factors beyond their control. Unintentional non-adherence occurs when patients genuinely want to follow the agreed-upon treatment plan but face obstacles that prevent them from doing so. These obstacles can include difficulties recalling or comprehending instructions, difficulties with treatment administration, financial constraints, or simply forgetting to take the medication.2
Understanding and distinguishing between these types of non-adherence is critical for developing effective patient adherence strategies. It’s important to note that improving medication adherence is a collective responsibility involving patients, healthcare providers, and healthcare systems. A one-size-fits-all approach is insufficient; rather, a multifaceted combination of adherence techniques should be employed to enhance a patient’s commitment to their prescribed regimen.5
To know about how adherence can improve health outcomes, read our article on Patient adherence: An opportunity for improving outcomes in neurologic diseases
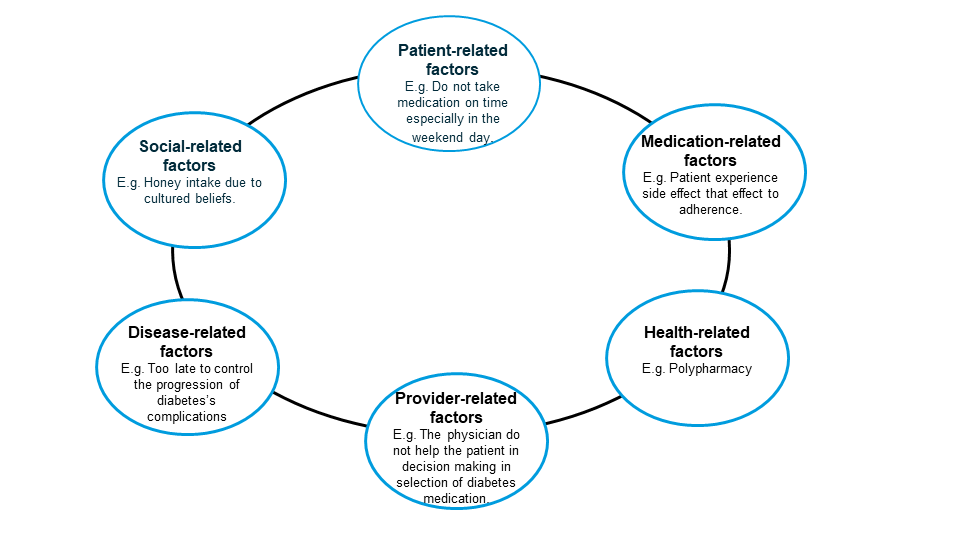
Barriers to adherence8
Figure adapted from Alodhaib, G et al. Pharmacy. 2021;9(1): 16.
Evaluating patient adherence: the foundation to improvement
Understanding the extent of medication nonadherence in patients is crucial for healthcare professionals, and it often goes underestimated. To tackle this, precise measurement and evaluation of adherence are essential.7 Self-reporting is an effective tool in this regard, as patients provide accurate information about their medication habits when asked directly.9-10
Various self-reported adherence scales have been developed to assess different aspects of a dosing regimen, including initiation, implementation, and discontinuation phases. These scales can be classified into five key categories: (i) those that solely evaluate medication-taking behaviors, (ii) those that assess both medication-taking behaviors and adherence barriers, (iii) those that focus only on adherence barriers, (iv) those that examine beliefs related to medication adherence, and (v) those that evaluate both barriers and beliefs affecting adherence.6
Besides comparing with other methods, self-report adherence scales can use average scores to set a clear cutoff for who is adhering to medication and who isn’t. However, some scales like the MAQ and MMAS prefer to rank how well people are following their medication plans instead of setting a fixed cutoff. These rankings can be based on actual health results or expert opinions.6
Moreover, the SPUR framework, along with objective methods such as electronic monitoring devices and pill counts, offer comprehensive and reliable data for adherence assessment.11
By utilizing these techniques, healthcare professionals can design effective strategies to enhance medication adherence and treatment outcomes. These tools serve as a strong foundation for optimizing patient adherence and ultimately improving patient care.12
To know more about different Tools to assess patient adherence read our article on Using tools to assess patient adherence
Also, read ‘Measuring adherence – an “Achilles heel” in medication adherence’ to know more about direct and indirect methods of adherence measurement
Improving medication adherence
Healthcare professionals play an essential role in improving medication adherence.13 Here are several strategies that can help:
Patient education: A crucial element for enhancing medication adherence is patient education; empowering patients increases their motivation to manage their condition and stick to their medication regimen. Another significant way to boost adherence is by actively involving patients in treatment choices, such as asking them their preferred time for taking medications.1
Provider-patient communication: The marked improvement in medication adherence among patients who have a strong rapport with their doctors underscores the pivotal role physicians play in this area. Effective communication is a cornerstone of a healthy doctor-patient relationship. Therefore, the most effective strategy for doctors to boost medication adherence may be adopting a patient-centered approach that encourages active patient participation in healthcare decisions, while also taking into account their cultural beliefs and attitudes.1
Simplified regimens: Complex medication regimens hinder adherence but simplifying them can enhance adherence. Claxton et al. demonstrated that once-daily regimens had significantly higher adherence compared to 3-times or 4-times daily regimens.14
Patient support programs (PSPs): PSPs provide tools such as education and reminders to support patients in managing their medication. They are effective in improving adherence through informational and behavioral strategies. PSPs aim to enhance patient engagement, disease management, adherence, quality of life, and communication with healthcare providers.11
To read more about PSPs, read our following article- The impact of Patient Support Programs on adherence: enhancing engagement and improving effectiveness
Use of digital technologies: Mobile phones, being the most widely used technology globally, offer a significant opportunity to impact large groups of people. Therefore, leveraging mobile health to improve chronic disease self-management, deliver health education, and enhance medication adherence could be a practical approach. Innovative tools like phone reminders, personal digital assistants, and smart pillboxes could be particularly helpful for patients struggling the most with adhering to their treatment plans.15-16
More information on how mobile apps can be used to enhance medication adherence, can be found in our other article, Mobile apps for enhancing adherence to chronic diseases
Interventions to improve medication adherence
Along with the above strategies, certain interventions have shown success in improving patient adherence:
Behavioral interventions: Behavioral interventions target altering specific daily life behaviors, and in the context of medication adherence, they focus on changing patients’ attitudes towards their treatment. These interventions often employ cognitive-behavioral methods and therapies aimed at addressing emotional, behavioral, and cognitive issues to encourage healthier lifestyles and positive treatment outcomes. However, the effectiveness of such interventions for improving medication adherence has been mixed. The most successful approaches are multi-component interventions, although they tend to be costly and challenging to integrate into routine clinical practice.17
Pharmacotherapy For patients on multiple medications, adherence improves with simplified regimens. Healthcare providers should aim for once-daily dosing, synchronize medication timing, and use combination pills when possible. If once-daily dosing isn’t feasible, aligning medication times with daily activities can help.18
Community pharmacy interventions: Community pharmacists, given their frequent patient contact, can help identify non-adherence and provide interventions, such as medication reviews and individual counselling.17
The role of healthcare providers in enhancing medication adherence
Physicians not only frequently overlook medication nonadherence in patients but may also contribute to it by prescribing complicated regimens, inadequately explaining medication benefits and side effects, and not considering the patient’s financial constraints. Poor communication, especially in chronic conditions like CVD, can further hinder a patient’s understanding of their disease and the importance of medication adherence. Additionally, not discussing alternative or herbal therapies can be another communication gap. Insufficient communication among physicians themselves can also exacerbate medication nonadherence. The healthcare system within which a physician operates plays a crucial role in achieving better patient health, and medication adherence is a key factor in this. Therefore, healthcare systems need to evolve to prioritize medication adherence, including making necessary changes to ensure that adequate time is devoted to discussing its various aspects.1
| Questions HCPs can ask in a blame-free environment to assess patients’ medication adherence1 |
| • These are difficult to take every day. How often do you skip one? |
| • There are quite a few medications; how many of these do you take? |
| • Most people don’t take all their meds every day. How about you? |
| • Have you stopped taking any of your medications when you feel well? |
| • Are you worried about any side effects from your medications? |
| • When was the last time you took drug A? Drug B? |
Improving medication adherence is a complex task that necessitates collaboration between healthcare providers and patients, innovative patient support programs, utilization of digital health technologies, and multifaceted interventions. By addressing individual challenges, we can significantly enhance patient outcomes and quality of life. As healthcare professionals, let’s continue the dialogue and strive for better adherence to drive improved health outcomes for our patients.1
“Were there none who were discontented with what they have, the world would never reach anything better.”
– Florence Nightingale












