Addressing mental health stigma to improve medication adherence
- Stigma is a trend highlighted by negative stereotypes and discrimination, has a significant impact on mental care, posing challenges to the prompt identification and treatment1.
- The negative impact of stigma in healthcare has led to call to action for health organizations, taking the lead in addressing the issue2.
- To overcome the stigma associated with mental illness, a multimodal strategy/intervention with education at its core is needed1.
- Low adherence to medication is attributed to several factors, including severity of illness, self-stigma, and negative attitude of patients3.
According to Global Burden of Disease (GBD) 2019 data, a large proportion of the disease burden is attributable to mental disorders with no evidence found in its reduction since 1990. Mental disorders accounted for 654.8 million estimated cases in 1990 which further exceeded 970.1 million cases in 2019, corresponding to an increase of 48.1%4.
Individuals with mental illness often face two significant challenges: coping with a wide range of symptoms and dealing with societal stigma associated with their condition5. The stigma of mental illness continues to be strong and pervasive in our society and has detrimental effects on people living with it5. This not only impedes individuals’ willingness to seek help but also influences their adherence to treatment plans, representing a tremendous burden on people with mental illness.
Understanding stigma in mental health
Stigma is defined as a complex social process of labelling, devaluation, discrimination, and othering2 that serve to distinguish individual from other members in a society. The concept of mental health is closely interwined with the concept of stigma2 as it manifests through a myriad of beliefs and negative attitudes leading to the social exclusion of individuals experiencing mental health problems.
This negative attitude can be categorized into three main types2:
- Intrapersonal (self-stigma)
- Interpersonal (relations with others)
- Structural (discriminatory and/or exclusionary policies, laws, and systems)
Individuals with mental health are deeply engaged with the social norms that can lead to delays in seeking treatment or outright avoidance, ultimately exacerbates the condition and complicates recovery1 (Figure 1). According to previous studies, the result shows that an increase rate of suicide is more likely due to public stigma of depression6. Self-stigma may inhibit individuals with a mental illness from seeking help7, interfere with medication adherence8, and provide barriers to their successful reunion within society9.
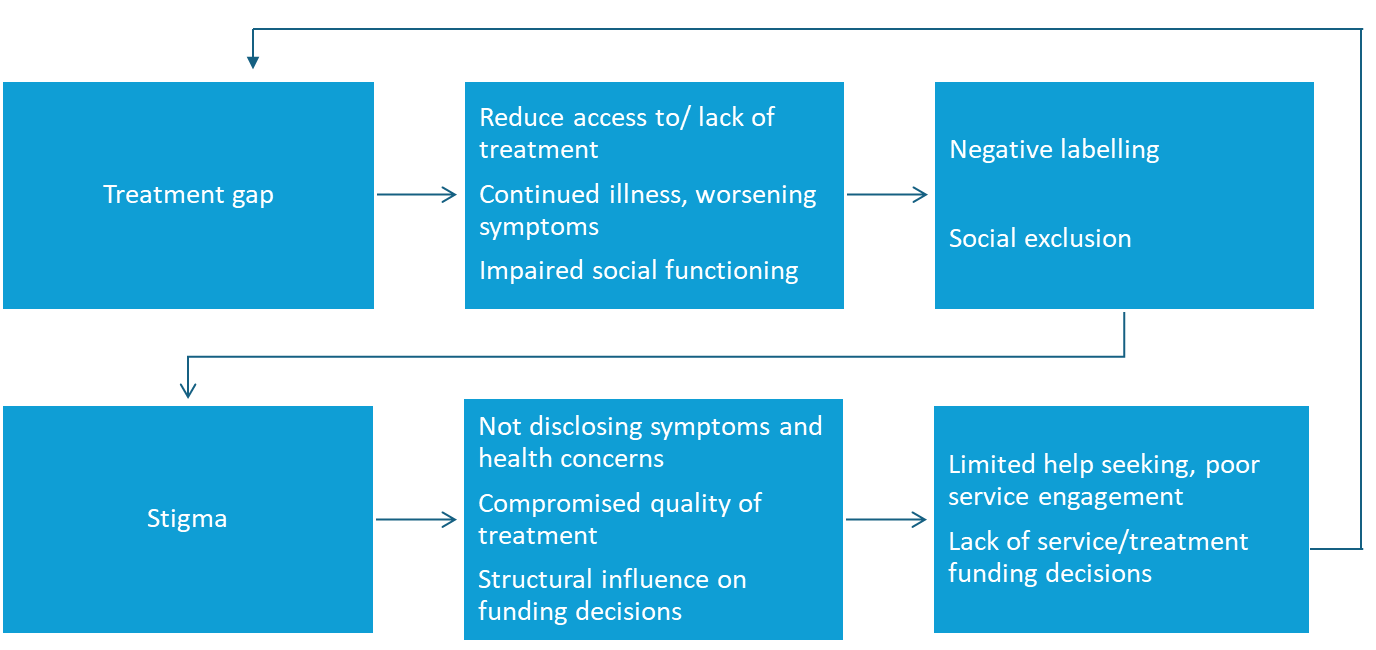
Figure 1: Exacerbation of treatment gap by stigma. (This figure is adapted from Gronholm PC et al., 2023)10
Non-adherence to treatment can be substantially impacted by stigma. It operates at various levels, and it can delay treatment-seeking1:
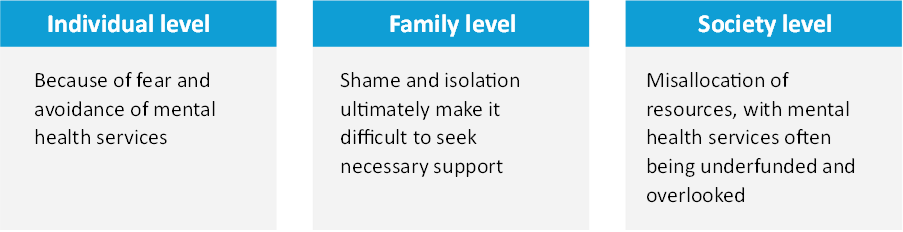
Individual and social perception of stigma in mental health
The way that mental health is interpreted in society has a significant impact on whether stigma will reduce or sustain. Media portrayals of people with mental health difficulties as dangerous, erratic, or unable to lead normal lives are key reasons behind increasing stigma and its effect on individuals as well as in society1.
Various barriers/perceptions that lies because of stigma in mental health includes:
- Reduced treatment adherence: Fear of recognition as a mental health patient leads to either outright avoidance or discontinuation of the ongoing treatment. This fear may worsen symptoms, leading to unsuccessful recovery, and increases relapse risk1.
- Delayed treatment-seeking behavior: The fear of being isolated or devalued due to mental illness often put off individuals from seeking professional help, worsen the symptoms and affect in different ways including self-care, less productive work, and relationships, hence reduce overall quality of life1.
- Social isolation/discrimination: Mental illness is often surrounded by certain social norms and negative stereotypes that result in lack of understanding and empathy from others, leading to feeling of exclusion1.
This discrimination can further complicate matters as it might affect individuals ‘attitude towards work, strain personal/professional relationships, friends and family may distance themselves due to discomfort, fear, or misunderstanding that exacerbate feelings of isolation and loneliness1. - Perpetuation of misconceptions: The persistence of stereotypes and false information that further impedes the public’s comprehension and acceptance of mental illness is a result of stigma and unfavorable attitudes toward mental illness. This, in turn, exacerbates stigma and has a detrimental impact on policy and legislation, which results in inadequate support and funding for mental health services1.
- Influence of gender on stigma: Stigma on mental illness varies between different social and demographic categories including gender which further influenced by cultural context1. Male experiences more burden of perceived stigma than women, reason reported as increased stress regarding disclosing mental illness as compared to women11. All these impact/portrayals reinforce negative stereotypes and misunderstandings about mental illness, making it more difficult for those affected to seek help and achieve successful recovery.
Stigma in healthcare
There are multiple sources of stigma in healthcare that directly or indirectly affect quality and access of care for the person living with mental illness.
- Negative attitude and behavior: Individual with lived experience are surrounded by stigma across the healthcare spectrum, including healthcare professionals with whom they contact to seek support2.
- Lack of awareness: Unconscious biases and lack of awareness are major factors in recognizing the influence of concealed attitudes and beliefs that can drive behavior associated with stigma2.
- Stigma in workplace culture: The issue is not limited to the outside world; stigma associated with mental illness also exists within the healthcare industry. It has been reported that this is a cultural issue since employees are frequently discouraged from seeking out help for psychological issues or talking openly2.
- Therapeutic pessimism and lack of skills: Due to lack of experience/skills, inadequate training and helplessness, healthcare providers hold this pessimistic view for mental illness which is another source of stigma2 (Figure 2).
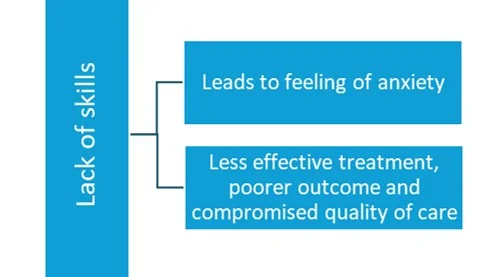
Figure 2: The impact of therapeutic pessimism and healthcare provider’s lack of skills on stigma in mental health (This figure was created for illustrative purposes and is based on data obtained from Knaak S, et al., 2017)2
Key approaches utilized to reduce stigma in healthcare settings1,12,13
- Provision of information: Teaching participants about the condition itself or about stigma, its manifestations, and its effect on health.
- Skills-building activities: Creating opportunities for healthcare providers to develop the appropriate skills; For instance, cultural competency training to value diversity, understanding cultural differences, and to care about organizational norms1,13.
- Participatory learning: This approach would lead participants to actively engage in the intervention.
- Contact with stigmatized group: To foster empathy, humanize the stigmatized person, and dispel preconceptions, this strategy depended on including members of the stigmatized group in the delivery of the interventions.
- An “empowerment” approach: To improve client coping mechanisms to overcome stigma at the health facility level.
- Structural or policy change approach: This approach includes changing policies, providing clinical materials, repair systems, and facility restructuring.
Also, a negative correlation has been seen between stigma and treatment adherence that is, the stigmatization affects the outcome of the disease by affecting the treatment compliance of individual with mental illness14; hence it is important to address the stigma to improve adherence in patients.
A study of group cognitive behavior therapy has shown to improve treatment adherence in major depressive disorder by reducing patients’ sense of stigma, and effectively alleviate depressive symptoms14.
To find more information on treatment adherence, please read our previous articles Improving treatment outcome in mental health by enhancing medication compliance and Medication compliance in mental health for improved treatment outcome
Strategies/Intervention to reduce stigma1
To combat the stigma associated with mental illness, a multimodal strategy or intervention with education at its core is needed. Some of the strategies include:
- Public awareness campaigns: Awareness campaigns can unmask mental health conditions and help to reach the unreached. This initiative may alter societal perceptions and reduce stigma by communicating facts about mental illness, their root causes, and their treatability1.
Various anti stigma campaigns have been shown to improve the negative attitude, using visual representation. For instance, “Time to change”, one of the largest campaigns for anti-stigma; launched in 2009. Data from this campaign has shown incremental improvement among the public to reduce stigma15. A systematic review showed that “media campaigns” revealed being a valuable approach, especially in preventing suicide by increasing knowledge and belief as well as modifying attitude towards it16. - Peer support program: Mental illness can be normalized, and stigmatization can be challenged by sharing real-life examples of patients who are managing their condition. By providing such experiences, peer-to-peer advocacy programs may debunk myths and reduce the perceived ‘otherness’ of mental illness1. A study using peer support has shown positive change in the mental health patients with acceptable means of exchanging information and belief on others for support17.
- Community-based mental health services: The stigma attached to obtaining psychiatric assistance can be addressed by integrating mental health services into community and primary care environments. By emphasizing the integration of mental health measures with other regular and standard primary care procedures, mental health care can be made more accessible and less scary, which in turn encourages people to seek help when they need it1. For instance, A program in India called the MANAS project integrated mental health into primary care and community settings that has not only made mental health services more accessible but also more ‘normal’ and less stigmatizing1.
- Evidence-based approach: Another approach to overcome the barriers created by stigma is to use evidence-based methods to reduce mental illness stigma1. In 2016, Corrigan PW in a meta-analysis mentioned that several evidence-based interventions, including education and contact-based interventions, might reduce mental illness stigma across cultures in an effective manner1,18.
- A study showed that using multi-method approach can serve as an effective model for implementing evidence-based psychological treatments for children with mental health needs with other chronic illnesses19.
- Another effective result was found by Diouf F, et al., by using evidence-based approach and implementing digital media campaign reduce stigma in different geographical locations20.
- A study showed that using multi-method approach can serve as an effective model for implementing evidence-based psychological treatments for children with mental health needs with other chronic illnesses19.
- Another effective result was found by Diouf F, et al., by using evidence-based approach and implementing digital media campaign reduce stigma in different geographical locations20.
- Multi-component interventions: Combination of various strategies simultaneously have shown to be more beneficial to reduce mental health related stigma, For instance, both media campaigns and educational intervention components or both educational and social contact strategies16.
- Local engagement and intervention exposure: Data from a systematic review revealed the positive effect of local engagement and intervention exposure and importance of local and community engagement for its effectiveness.
In several nations, institutional and organizational stigma connected to mental health has been significantly lessened or mitigated by the implementation of public policy measures. For instance, the 1990 Americans with disabilities act in the US mandated the social inclusion and involvement of people with mental health concerns in society, as well as the prevention of discrimination based on mental health21. This was followed in 1999 by a report “Mental health: A report of the surgeon general”, which aimed to educate the public about stigma and discrimination related to mental illness. In addition, the mental health services act of 2004 in California tackled stigma on an institutional, societal, and personal level through training, social marketing, and an emphasis on cultural competence21.
Conclusion
Stigma in mental health is a complex and multifaceted issue that varies across various contexts. It can also lead to non-adherence to treatment. In addition, of having an adverse emotional impact on treatment outcomes, stigma and non-adherence also force patients to mask incorrect behavior, which may exacerbate symptoms. It is imperative to design culturally appropriate interventions and to promote awareness and acceptance of mental health conditions to successfully address and reduce stigma at various levels including mental healthcare settings. By doing this, we can endeavor to enhance the availability of mental health services and advance the well-being of people and communities worldwide.
“We need so much more openness, transparency and understanding that it’s OK to talk about depression as an illness. It’s not a weakness. It’s not a moral shortcoming. It’s not something people brought on themselves”.
– JOHN F. GREDEN