Medication compliance in mental health for improved treatment outcome
- Mental illness is a common health issue that results in partial to complete disruption to a patient’s life1,2.
- Albeit common, it is stigmatized in the community, and adherence to psychotropic medication is poor as patients often suffer in secret3.
- Non-compliance to medication in mental health is majorly caused by patient-related issues like poor disease insight, negative attitude towards psychotropic medications as well as other social and system-related factors3.
- Psychotropic medication non-adherence can be best addressed by using combinatorial interventions with a scope of long-term follow-up and repetitions4.
Good health is defined as a state of physical, mental, and social well-being. Lack of debilitating physical symptoms alone doesn’t necessarily mean sound health. Although the focus on mental health is growing, the global efforts to remedy them have remained insufficient1. Mental health conditions include various mental and neurological disorders, substance-abuse behavior, suicidal tendencies as well as intellectual and cognitive disabilities5.
“Mental illness is not binary or exclusive, but rather complex and universal. It can be best described as a spectrum, at one end of which is mental health where people are thriving and are at ease. In the middle reaches are people who are coping, surviving, or struggling. While at the far end of the spectrum sits all the mental illnesses. Patients move back and forth along the spectrum their entire lives” – as described by Mark Rice-Oxley, The Guardian’s executive editor6.
Mental illness – a silent epidemic
Mental illnesses are called silent or hidden epidemics due to the stigma and secrecy that surrounds them. Globally, one out of every 8th person is struggling with some type of mental health challenge resulting in 1 in 5 years lived with a disability1,7. Mental health issues make up 14% and 30% of the global burden of diseases and non-fatal disease burden, respectively. One-third of psychiatric patients suffer from near-permanent disabilities and require long-term care3. With more than 450 million people affected globally, it causes several trillions of dollars in losses annually due to reduced productivity and premature mortality3. The major mental health issues are classified into the following categories5:
- Depression
- Anxiety
- Bipolar disorder
- Post-traumatic stress disorder
- Schizophrenia
- Eating disorders
- Disruptive behavior and dissocial disorder
- Substance-related addictive disorders
- Sleep-wake disorders
- Neurodevelopment disorders
- Neurocognitive disorders
Various factors like biological, social, environmental, and structural issues can exacerbate or resolve a mental health issue2,3. Mental health is a significant challenge during the formative years of adolescence and young adulthood contributing to 13% of the disease burden. The hormonal changes along with parental pressure, peer discordance, socio-economic issues, identity exploration, and exposure to violence are the primary cause of mental illnesses like depression, anxiety, behavioral disorders, and suicidal tendencies in this age group. Evidently, suicides are the fourth-highest cause of death in adolescent-young adults8.
Mental health well-being – a global challenge
Sound mental health is required for coping with everyday stresses and for being productive to one’s full potential. It is also essential for day-to-day as well as complex decision-making2. Good mental well-being has been accorded the status of a basic human right and is pivotal for personal and socio-economic development2.
Realizing the importance of mental health, WHO has begun a global initiative to raise mental health awareness in 12 priority countries to ensure affordable quality care for 100 million people by 2023 through its special initiative – Univeral Health Coverage for Mental Health. The specific goals for this special initiative are1:
- Advancing policy and advocacy for mental health.
- Scaling interventions to address mental illnesses in different healthcare settings.
The last decade has seen the destigmatization of mental illnesses. Even though people are more vocal and concerned about their mental well-being, psychiatric patients are still discriminated against and suffer human-right violations. Both patients and family members seem to be resistant to the idea of accepting their health condition. Even with the availability of comprehensive treatment, non compliance with medication in mental health is common resulting in poor disease outcomes3.
Medication adherence in psychiatric patients– why it Matters?
Patients suffering from mental illnesses are especially prone to non-adherence to medications due to a lack of insight about either their mental health status or the necessity of the treatment. For more on how the lack of disease insight impacts medication adherence in severe psychotic disorders, please read our article “Non-adherence in patients with schizophrenia: An issue of impaired insight” and “Severe psychiatric disorders: causes & interventions for medication non-adherence”. Therefore, non-adherence to psychotropic medications for mental illnesses can result in3,
- Exacerbation or relapse of symptoms and poor prognosis
- Reduction in treatment efficacy
- Less responsive to second-line psychotropic medications
- Increased hospitalization
- Poor psycho-social outcomes
- Enhanced suicidal tendencies
- Higher risk of co-morbidities
- Wastage of resources
- Higher economic burden on patients
- Enhanced burden on the healthcare system
Rate of non compliance with medication in mental health
A recent systematic review of more than 45 studies from all the major geographical regions estimated the overall levels of medication compliance in psychiatric patients for the major mental disorders (Schizophrenia, bipolar disorders, and depressive disorders) to be only about 49% 3 (Figure 1). On similar lines, another study reported low rates of persistence to psychotropic medications with about 25% of patients discontining their medications within the first week of treatment initiation4. The rates of psychotropic medication non-adherence also varies between different geographies (48-57% )3.
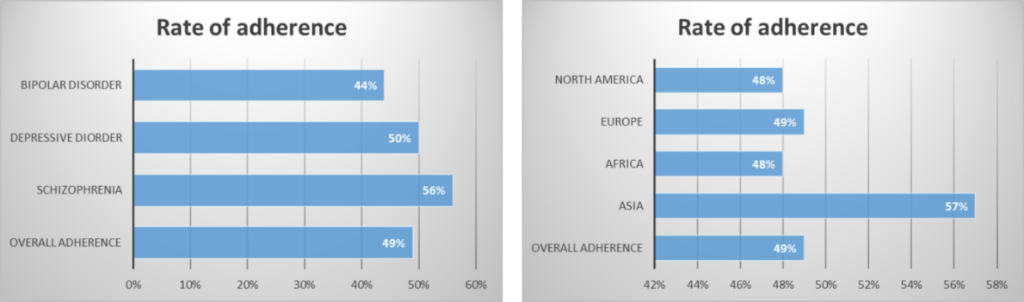
Figure 1: Rate of adherence to psychotropic medications for major psychiatric disorders in different geographical regions3.
Determinants of non compliance with medication in mental health
As detailed in our other articles on metal illnesses like schiziophrenia and other severe psychotic disorders, several determining factors exist for non-adhering to psychotropic medications – some are the root cause of the non-adherence while other exacerbates it. These factors are grouped into three categories3
- Patient-related: perceived stigma, lower priority to mental health, attitude towards medication, low necessity belief, impaired insight about the disease
- Medication-related: side-effects, duration of therapy, the complexity of regimen, medication efficacy, costs, relapse of symptoms3
- Health-system related: unavailability of medications, patient-provider relationship, lack of mental health facilities and trained workforce10
- Social factors: socio-demographic factors, disease-related-stigma, lack of social and family support
Are interventions to improve psychiatric medication compliance effective?
Various interventions have been designed and implemented for alleviating non-adherence to psychotropic medication. As mentioned in our other article on severe psychotic disorders, the interventions to enhance adherence to psychotropic medication can be categorized as follows:
- Educational interventions
- Behavioral (cognitive) interventions
- Therapeutic alliance with healthcare practitioners.
- Technological interventions
- Combinatorial interventions
Effectiveness of behavioral interventions:
A meta-analysis of various interventions aimed at improving non-compliance with medication in mental health reported significant gains using behavioral interventions. All such studies successfully employing behavioral interventions used a personalized approach to suit patients’ individual needs. They used daily SMS reminders, motivational interviewing, home visits, and training to enhance self-efficacy in patients. Studies using SMS to deliver behavioral interventions and reminders or using motivational interviewing reported a significant enhancement in medication adherence in psychiatric patients as compared to the control group receiving standard care. On the other hand, strategies using SMS or phone calls aimed at problem-solving or cognitive behavioral therapies failed to modify adherence behavior4.
Effectiveness of educational interventions:
Personalized educational interventions aimed at enhancing general health awareness or providing specific disease- or/and medication-related information were also successful in medication compliance in psychiatric patients. The personalized interventions included either one-on-one interaction with the health care professional or small group therapies. These sessions involved delivering information about the nature of the disease, expected symptoms, the role of medications, and medication adherence as well as interactive Q&A sessions for encouraging patient-provider interaction. Interstingly, the educational interventions centering on stress management and enhancing problem-solving skills did not produce a positive effect on medication adherence4.
Effectiveness of combinatorial interventions:
Combinatorial interventions are known to be more effective than any one individual intervention for enhancing adherence. Along similar lines, studies focusing on psychiatric medication compliance reported improved medication adherence using a combination of motivational interviewing and educational strategies for both patients and caregivers. Albeit, a combination of cognitive behavioral therapy and motivational therapy was found to be ineffective4.
Strategies to improve medication adherence in psychiatric care
- Combinatorial and personalized interventions:
The barriers to adherence vary considerably and therefore a combinatorial approach is essential. Behavioral interventions like PharmCAT and Med-eMonitor incorporate electronic devices and a personalized bouquet of interventions (signs, alarms, checklists, tailored information, pill containers, etc.) to suit patients’ specific needs4.
- Repetition and adequate follow-up:
Non-compliance with medication in mental health is a persistent issue and patients are prone to relapse. Therefore, repeating the intervention and routine follow-up is necessary. Analysis of results from studies reporting different time durations – 6, 12, and 24 months – of follow-up suggests that interventions designed for shorter durations work well and positively impact adherence similar to long-term interventions. Non-adherence is a recurrent behavior and therefore it requires booster sessions to avoid relapse4.
- Using multiple methods to assess adherence
No single method to assess adherence can measure the behavior adequately (please read Measuring adherence – an “Achilles heel” in medication adherence) Therefore, two or more assessment methods (pill count, serum levels, adherence questionnaires, etc.) suited to the patient’s need are essential to confidently measure adherence behavior4.
- Building a trusting partnership between patient and practitioner
Above everything else, a trusting partnership between the patient and the healthcare practitioner is pivotal for the success of any given therapy. This is even more important in psychotherapy since its success is often influenced by the positive treatment environment and the positive perceptions of the patient11.
For more on this read our article “healthcare practitioners: a potential springboard for adherence success”.
Conclusions
Enhancing medication compliance in psychiatric patients requires a concerted effort from patients, caregivers, and healthcare providers in addition to a positive attitude from the community towards mental illnesses. Better strategy is to use multiple methods of assessment and a combination of interventions. The interventions should have a long-term follow-up built into the approach and should be repeated at regular intervals for consistent gains in adherence behavior4.
“Unfourtunately, I think depression and anxiety are really hard to live with. And what people dont need is to feel bad about themselves because they decide to go on medication.” – Rene Russo (American actress/model and a patient of bipolar disorder). Source: ABC news 2014