Innovative drug delivery: Can it deliver on the promise of medication adherence ?
- Medication non-adherence is majorly addressed by patient-centric interventions by providing health education, behavioral interventions, and improving patient-provider relationships1,2.
- Use of innovative drug delivery systems is an alternative approach to enhance adherence by reducing dosing frequency, minimizing adverse effects, and improving treatment efficacy3,4.
- Innovative drug delivery systems offer enhanced efficacy, lower side effects and better patient comfort increasing patient adherence3,4.
Improving medication adherence is touted to have a greater impact on treatment outcomes than the improvement in any one specific treatment. However, it remains a formidable challenge due to its multifaceted nature impacting population health, quality of life, and health economics2.
Barriers to non-adherence are multifactorial and dependent on factors such as2,
- Patient-related factors
- Social/economic factors
- Health system/HCT – factors
- Therapy-related factors
- Condition-related factors
Conventionally, interventions to address non-adherence aim to alleviate patient or physician-related barriers through patient-centric approaches such as improving patient-health provider communication, behavioral interventions, providing health education, and medication reminders2. To learn more about interventions for improving adherence, please read our other article “Interventions to tackle medication non-adherence”. However, these approaches have shown inconsistent and underwhelming results and are not adequately effective in improving adherence3. Strategies that target medication-related barriers such as innovative drug delivery systems are promising tools with the potential to enhance medication adherence by enhancing performance, convenience, and patient compliance 3.
Drug delivery systems
Drug delivery systems (DDS) are the drug carriers or transporters fabricated using advanced technology, systems, or formulations to facilitate the delivery of drugs to specific cell/tissue types as well as regulate their release in the body over time to maximize therapeutic efficacy and minimize off-target effects. These systems help in keeping the medication concentration within the required therapeutic range without the futility of systemic exposure3,4.
Innovative drug delivery systems aim to enhance the pharmacokinetics of an active pharmaceutical ingredient by slowing down or allowing periodical/sustained release as well as facilitate different routes for delivery. The routes of drug delivery could include oral, buccal, sublingual, nasal, ophthalmic, transdermal, subcutaneous, anal, transvaginal, or intravesical4. Consequently, this may lead to improved efficacy as well as a reduction in the dosage frequency, adverse effects, and toxicity4. Drug delivery systems (DDSs) can also benefit patients feeling stigmatized or embarrassed in regularly visiting pharmacies for prescription refills and allow for added discretion. These improvements can help overcome multiple drug-related barriers to adherence3.
Drug delivery systems – Old versus New
Possibilities for modulating drug release have been explored since the 1950s when the first oral sustained-release formulations were developed by layering the active ingredient alternatively with coats of enteric polymers. These were then followed by the development of first and then second-generation DDSs such as nanoscale drug-polymer conjugates, liposomes, microspheres, nanoparticles, pH/temperature-responsive SMART polymers, etcetera4. Technological advancements have led to the development of the third generation of DDSs with the potential to offer better efficacy and precision largely due to,3,4.
- Enhanced permeability, solubility and stability
- Novel drug release profile – Sustain/prolong/pulsatile, first/zero order, stimuli-response drug delivery
- New routes of administration – oral, transdermal, intravenous, intramuscular, subcutaneous, transmucosal
- Smaller particle size
- Lower toxicity
- Higher cell/tissue-specificity
Innovative drug delivery systems
Merging innovations in various biomaterials, nanotechnology, 3-D printing, implantable devices, RNA therapeutics, and artificial intelligence has heralded a transformative era in drug delivery that offers higher precision, controlled release, enhanced patient compliance and data-driven personalizion of treatment plan5.
Nanocarriers used in the delivery of drugs can be nanoparticles made of organic or inorganic or hybrid polymers, liposomes, micelle, or dendrimers6.
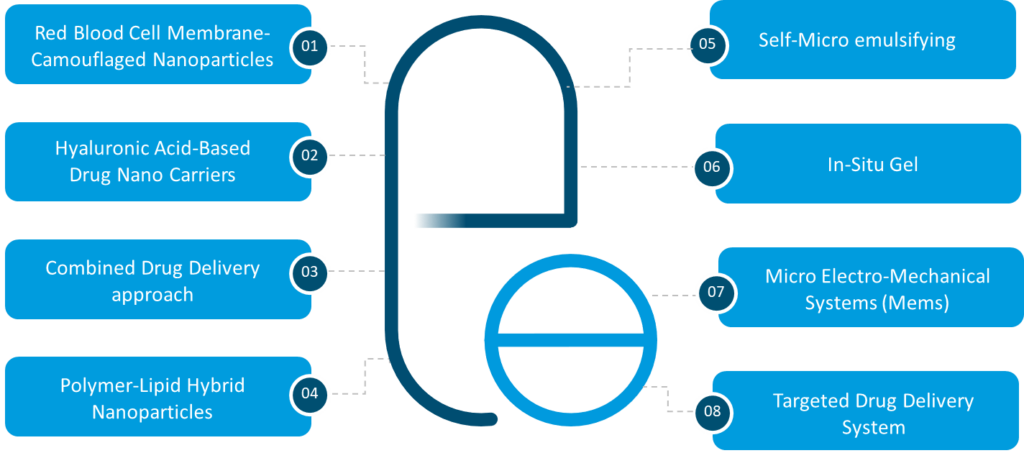
Figure 1: Various types of advanced drug delivery systems4. (This figure was created for illustrative purposes and is based on data obtained from Ezike et al., 2023)
Some examples of these innovative systems include4:
- Red blood cell membrane-camouflaged nanoparticles: Nanoparticles camouflaged with red blood cell membranes are a novel class of nanocarriers. The nanoparticles loaded with the drug are fused with RBC membranes via processes like sonication or microfluidic electroporation. The unique coated surface imparts biocompatibility and extended circulating half-life of RBCs to the delivery vehicle4.
- Hyaluronic-acid-based nanocarriers: Hyaluronic acid is a high molecular weight polysaccharide abundantly present in our extracellular matrix especially in connective tissues. It is a popular choice for carrier systems such as those using the ocular mode of delivery due to its biocompatibility, biodegradability, high viscoelasticity, and natural abundance in the eyes4.
- Polymer lipid-hybrid nanoparticles: Liposomes and polymer-based nanoparticles are one of the most popular drug delivery systems in use. Liposomes are lipid-biomembrane mimics with excellent biocompatibility but marred with instability and leakiness. On the other hand, polymer-based nanoparticles are extremely stable but have lower biocompatibility. Polymer lipid-hybrid nanocarriers combine the best of liposomes and polymeric nanoparticles4.
- Self-microemulsifying systems: Lipid-based carrier systems enhance the bio-availability of hydrophobic medications. Self-emulsifying lipid carriers can incorporate the hydrophobic drug and sustain them in solution all through the digestive system4.
- Targeted drug delivery system: An advanced technique to enhance efficiency and reduce side effects by delivering the drug in a targeted manner to specific cells/ tissues by attaching antibodies or ligands to drug carriers. This approach increases drug concentration at the target site4. This approach utilizes diverse drug carriers like soluble polymers, biodegradable microsphere polymers, neutrophils, liposomes, micelles, and artificial cells. It proves particularly valuable in cancer treatment, enabling optimal therapeutic effects with reduced material in a well-controlled manner4.
- Controlled-release drug delivery system: This drug delivery system follows a non-invasive and controlled-release approach, bypassing the first-pass metabolism. They have been designed to release medication slowly over a particular period, ensuring a consistent therapeutic effect and less frequent dosing. Transdermal patches, in-situ gels, microneedle patches, and implantable devices offer sustained release, enhanced patient comfort, and compliance3,5,6.
- Combined drug-delivery approach: A major barrier to non-adherence is administering multiple medications several times a day. A technology that combines multiple compatible medications in a single pill can help in this aspect. Combined drug delivery also helps in overcoming muti-drug resistance with a reduction in dosage and adverse effects4.
- Gene, RNA-based therapies, and 3D printing: Gene and RNA-based therapies have now opened new opportunities for drug delivery. lipid nanoparticles and viral vectors are widely used to deliver genetic material to specific target cells. 3D printing has also revolutionized the manufacturing of drugs and personalized medicine. This technology has enabled the manufacturing of customized drug formulations modified according to individual patient needs6.
Addressing Non-adherence challenges:
Innovative drug delivery systems offer various benefits that have the potential to address medication-related impediments to treatment non-compliance. Some of these are discussed below in detail:
- Simplified regimens: Taking medication once a day is preferred by many patients. Extended-release formulations and different implantable devices reduce the dose frequency, making it easier for patients to adhere to their treatment regimens. Study shows that adherence rates among patients taking medications once a day were significantly higher than the rates among patients taking medications twice a day or thrice a day. Less frequent administration also reduces the risk of repeated exposure to high drug concentrations, which can give rise to short-term adverse effects, and increased risk of developing resistance, tolerance, and physical dependence on the medication3.
- Convenient dosing through single-pill combinations: Chronic diseases require patients to take multiple medications more than once a day to manage their condition leading to confusion and unintentional missed doses. Drug delivery systems that combine multiple compatible medications in one single pill can be effective in enhancing adherence and persistence to the regimen as reported in patients on antihypertensive treatment7.
- Avoiding first-pass metabolism and the increased onset of action: Using a parenteral route- such as subcutaneous, intravenous, transdermal, intramuscular, sublingual, or, intranasal administration- avoids first-pass metabolism which delivers the drug directly into the bloodstream or the targeted site. This approach achieves the same therapeutic effect and enables a faster onset of action in comparison with oral drug delivery. This can increase patient adherence as the effect is immediate with fewer symptoms3.
- Mitigation of adverse effects: Medication-related adverse effects are a major hindrance to patient medication adherence. Targeted DDS that delivers medication to specific cell/tissue types has the potential to substantially reduce multiple types of treatment-emergent adverse effects by avoiding systemic exposure to the drug4. Similarly, long-acting formulations of the drugs instead of short-acting formulations can reduce the frequency of side effects. These targeted or extended-release formulations can have improved tolerability thereby improving the quality of life and can minimize the number of delayed or missed doses caused due to experiencing adverse effects3.
- Reduced pain: Phobia with needles can be a major cause of non-adherence to patients. Nasal and oral vaccines can be possible alternatives to intramuscular vaccines with a hypodermic needle to increase patient compliance and medication adherence. Transdermal microneedle array patches (MAPs) deliver drugs to the upper dermis or epidermis, avoiding the cutaneous pain receptors, and allowing for painless drug delivery3.
- Increased cost-effectiveness: Innovative drug delivery systems have shown the potential of reducing the total drug amount that is required to achieve a therapeutic effect by controlling and managing the systemic concentration of the drug and its rate of clearance3. Extended-release drug formulations can minimize the need for frequent administration by physicians, leading to fewer doctor visits and lower costs. They also offer the potential for storage outside the cold chain and/or self-administration, reducing costs and enhancing accessibility3.
- Destigmization: Disease-related stigma is a key barrier to medication adherence. Slow-release and long-acting formulations that reduce the dosage frequency can help in non-adherence due to disease-related stigmatization3.
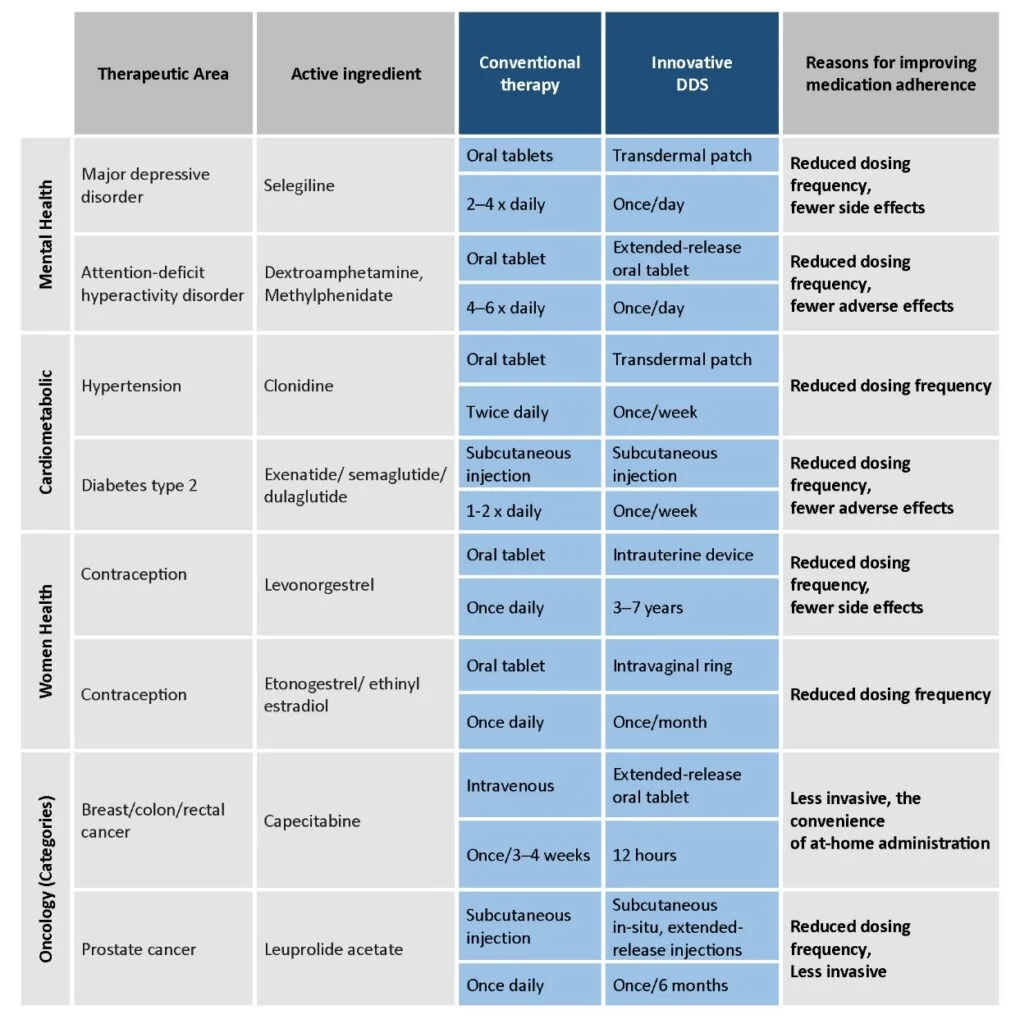
Table 1: Benefits of innovative drug delivery systems in improving medication adherence as compared to conventional drug formulations in key therapeutic areas3.( This table was created for illustrative purposes and is based on data obtained from Baryakova et al., 2023)
Conclusions:
The science of delivery of drugs has come a long way from old traditional methods to novel targeted approaches. This evolution has reshaped the landscape of the healthcare system, offering a new hope for more effective treatments with fewer adverse effects3. Innovative drug delivery systems promise to address the drug-related barriers and challenges of medication adherence. By focusing on alternative routes of drug administration, reducing the frequency of dose plus overall costs, and enhancing convenience, these novel technologies have the potential to improve treatment compliance and ultimately enhance the quality of life for patients with chronic conditions3. As technology is at the revolutionizing stage, one may expect a future where drug delivery can be truly personalized.
The doctor of the future will give no medication, but will interest his patients in the care of the human frame, diet and in the cause and prevention of disease.”
~ Thomas A. Edison












