Non-compliance in heart failure patients- an emerging pandemic
- Heart failure is an emerging epidemic due to an increase in life expectancy and better treatment outcomes for various cardiac ailments 1,2.
- Prevalent in older populations (>80% of patients above 65 years) suffering from multiple co-morbidities, the treatment management is often challenging due to lower rates of persistence to therapy3-5.
- Use of medication counseling, health education, and behavioral interventions have reported significant reductions in non-compliance in heart failure patients6.
Introduction
Heart failure defined as a chronic functional impairment of cardiac muscles is a life-threatening public health issue. It is an “emerging endemic” affecting more than 64 million people worldwide1,2. In high-income countries, the prevalence of diagnosed heart failure in the general population is estimated to range between 1-2% and could be as high as 11.8% in the older population ( >60 years). Also, evidence indicates that heart failure is on the rise in low-income countries1,2.
The prognosis of heart failure remains remarkably poor around the globe, particularly in middle-low-income countries. Over 80% of heart failure patients are older than 65 years of age making disease management challenging and resulting in high hospitalization and re-hospitalization rates3. As heart failure is a chronic condition, its clinical management requires strict long-term use of multiple drugs with a compliance rate of >80% for optimum therapeutic efficacy 4,5.
Rates of Non-compliance to heart failure medications:
Non-adherence to heart failure medications is a significant problem and the rate of noncompliance is reported to increase with age3. Current data suggest that ~ 25% of patients with heart failure are not consistently adherent to their prescribed medications, ~50% of chronic heart failure patients consume inadequate dosages of medications, and 30-50% of patients are said to be nonadherent to heart failure medications7,8. A large Danish study monitoring medication adherence in more than 100,000 heart failure patients post-hospitalization revealed decreasing rates of persistence to different heart failure medications in the population over a period of 5 years9 (Figure 1).
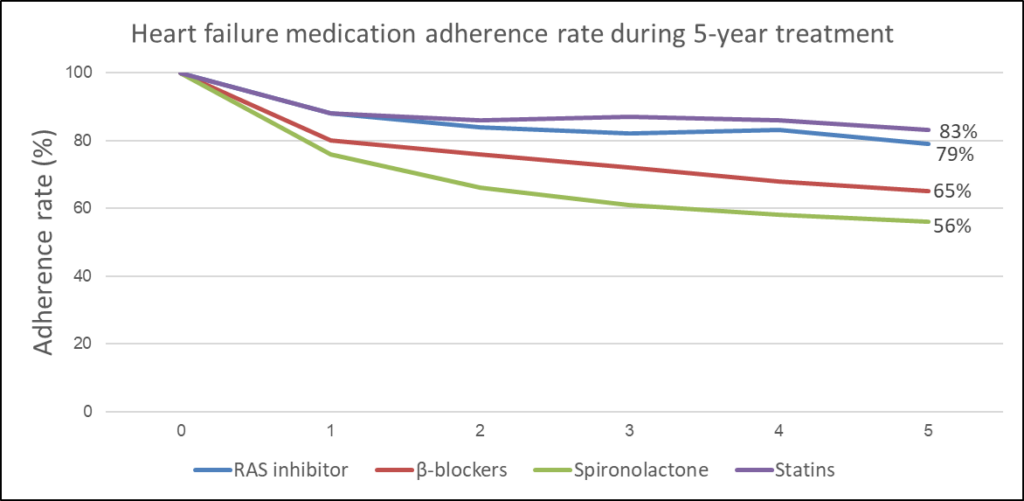
Figure 1: Rate of medication adherence to different heart failure medications in patients 5 years post-hospitalization. RAS: Renin–Angiotensin System (adapted from Gislason et al., 20079).
Effects of non-compliance on heart failure patients
Medication compliance in heart failure patients helps in managing symptoms, improving clinical outcomes, and reducing the associated mortality7. Although, heart failure is primarily a disease of the older population, recent data points towards an increasing heart failure burden towards the young population due to unhealthy lifestyles and a rise in obesity1.
The two major impacts of noncompliance in heart failure are:
- Increased hospitalization– Heart failure is the most common cause of hospitalization for patients older than 65 years of age3 and low compliance in heart failure patients has been linked to frequent cardiovascular-related emergency department visits and inpatient hospital days4. Research suggests that non-adherent patients constituted 22.1% of all hospital admissions associated with heart failure and after first hospitalization for heart failure, ~25% of patients are re-hospitalized within 30 days, and ~50% are re-hospitalized within six months3,7.
- Increased mortality- Medication non-adherence is a known predictor of early mortality5. Heart failure patients with medication nonadherence were 1.86 times more likely to experience a cardiac event than those with better medication adherence10 and non-adherence to β-blockers had around a 40–50% higher risk of death due to heart failure11.
Factors causing non-compliance in patients with heart failure.
The causes for medication non-compliance in heart failure can be patient-related (gender, age, education, socioeconomic), disease-related (multiple comorbidities), regimen-related (medications cost, adverse effects of medications, pill burden), or healthcare provider-related7,12:
- Age: The prevalence of heart failure is majorly associated with old age (0.04% in 18–44 years vs. 20.9% in ≥85 years). Age-related visual, hearing, cognitive, mobility, and swallowing impairments are evident challenges of compliance in heart failure patients13.
- Comorbidities: Non-compliance to medications in patients with multiple comorbidities is in general low. Heart failure patients are known to suffer from other comorbidities like chronic obstructive pulmonary disorder (24.1%), diabetes mellitus (34.7%), hypertension (52.7%), anemia (10.9%), and, renal function disorder (61.8%)13.
- Psychological factors- A patient’s psychological status, ability or motivation to adhere to prescription, use of drugs or alcohol, as well as necessity vs. concern beliefs towards therapy impacts adherence14. Depression is one of the most prevalent psychological complications in heart failure patients leading to non-adherence15.
- Therapy-related factors- Medication-related factors affecting non-compliance in cardiac patients are substantial. Medication side effects, regimen complexity, frequent regimen changes, and longer duration of regimen are the reasons for lower adherence and medication discontinuation in heart failure14.
- Socio-economic factors- A lower family/social support, economic status, and health literacy are associated with medication non-adherence among patients with heart failure. Additionally, different cultural beliefs also result in higher non-adherence to medication in the older population suffering from heart failure14.
- Healthcare provider and healthcare system–related factors: Poor patient-provider relationship and communication as well as difficulties in accessing pharmacies or healthcare facilities are also major causes of non-compliance in heart failure14.
Interventions for medication non-adherence among patients with heart failure
Although non-compliance in heart failure patients is high, timely and appropriate interventions can improve adherence rates and lead to better disease outcomes with reduced mortality. A systematic review of intervention studies has reported significant reductions in mortality risk (RR 0.89; 95% CI). and hospital readmission (OR 0.79; 95% CI) in heart failure patients16.
Interventions used for enhancing adherence in heart failure patients are described below. Several studies test a combination of these interventions to enhance adherence.
- Behavior interventions: Behavioral interventions based on different behavioral models and theories have been in practice to change medication-taking behavior. A study using interventions based on the “Theory of Planned Behavior”(TBP) reported improvement in adherence to therapy and clinical outcomes of heart failure patients when compared to the control group17.
- Medication reminders: The current digital technology market provides a wide range of digital devices that have in-built automated reminder systems. Medication reminders such as phone reminders, automated SMS reminders, and reminder pillboxes are in use to enhance adherence to heart failure medications. Studies have also shown the effectiveness of using a reminder book in HF patients for enhancing therapeutic adherence6,18.
- Health Education: The health literacy of patients has been a strong predictor of medication compliance in heart failure patients, while lower health literacy has been associated with poor self-care standards. A study using patient education and counseling sessions conducted by nurses for 2-3 weeks post-hospitalization improved adherence in the intervention group (P<0.0001) as compared to controls6.
- mHealth: Mobile phones are a promising tool for delivering healthcare interventions and can be used to educate, monitor as well as enhance adherence. A study using telehealth (using an ePill box) and mHealth in heart failure patients observed overall adherence rates of 78% in the intervention group. Although there were no significant differences between the two intervention arms, the patients preferred the mHealth approach19.
Multidimensional solutions involving two or more above-mentioned interventions tailored to the needs of patients are more likely to work. Table 1 describes a few such interventions and their effect in enhancing adherence6
Table 1: What works and what doesn’t for improving compliance in heart failure patients6.
| Intervention | Adherence Measurement | Results |
| Personalized education and counseling | Brief Medication Questionnaire | The intervention group had higher levels (p < 0.001) of medication adherence |
| Home communication intervention devices | Cardiovascular Risk Factor Modification Adherence | No statistically significant differences between groups |
| Regular audio- and video- call reminders | MEMS® caps | No statistically significant differences between groups |
| Smartphone application, pillbox | Bin opening or self-report on app | Device type not associated with medication adherence |
| Medication counseling, calendar, and medication information through pharmacist | Tablet count | The counseled group had statistically higher (p < 0.001) compliance |
| Matching icon on medication bottle and instruction sheet, written and verbal education through pharmacist | MEMS caps and refill adherence medication possession ratio | The intervention group had a statistically higher (p < 0.007) refill adherence |
| Teaching, medication simplification, and regular HCP contact after discharge | Pill count | The intervention group had statistically higher (p = 0.003) medication adherence than the control group |
| Education, diary cards, and medication simplification | Self-report | The intervention group had statistically higher (p = 0.039) medication compliance |
The way forward:
Digital health technologies have immense potential to provide personalized care, thereby improving patient–provider relationships and enhancing medication adherence. Benefits for patients include improved health literacy, self‐monitoring, and increased compliance, thereby empowering patients to take a more active role in their care. Bodyport (a “smart” scale that measures clinically relevant markers of fluid and cardiovascular status), Conversa (an automated conversational platform designed to engage patients in self‐management), and Noom (a smartphone coaching application that uses evidence‐based behavior change techniques to coach patients towards better self‐management of their syndrome) are some examples of digital health platforms for heart failure patients that can help in improving non-compliance. Although these technologies provide promising benefits and advantages, they also face multiple challenges in clinical workflow, enhancing physician burden, and difficulty in use20.
Conclusion
Noncompliance with medication is a major challenge across the healthcare system. In chronic conditions like heart failure, ~30-50% of the patients are non-adherent due to various contributing factors. Interventions currently in use have provided mixed results concerning improvement in non-compliance in heart failure patients. The development of patient-centered adherence solutions as well as upcoming technological advancements such as mobile devices and sensors hold immense promise for the future21. However, the focus should be on adapting these technologies for the older age group that forms the majority patient group and is often resistant to technological advances. Also, the increasing prevalence of heart failure in middle-low economic countries needs to be considered while designing the interventions for its widespread application.
“Heart disease is not a death sentence; it’s a wake-up call.”
– William Marks












