Understanding adherence from a cardiovascular-disease perspective
Key Messages
- Adherence is a behavior that encompasses the patient, the healthcare provider and the ability to follow agreed recommendations e.g., dietary changes and exercise
- Adherence comprises multiple stages and can be divided into intentional or non- intentional behaviors
- There are a variety of factors that influence one’s ability to adhere, extending from the initial consultation through to a societal level
Defining adherence
Adherence is a key factor in the effectiveness of therapies for both chronic and acute diseases. This is particularly true for cardiovascular disease, where nonadherence to chronic medications can have a negative impact on both the patient and the healthcare system. Non- adherence is often dubbed the Achilles heel of evidence-based medicine, as patients who don’t adhere as prescribed will fail to reach clinical goals and have suboptimal clinical outcomes, and the true impact of the medication remains unknown or unclear.1
The definition of adherence has evolved since the initial 2001 WHO description of, ‘the extent to which patients follow medical instructions’. While this was a helpful starting point, it did not encompass the range of medical interventions used to treat chronic diseases. This evolved further to overcome the passive nature of the patient; where patient behavior towards adherence is reflected in multiple stages: filling prescriptions, taking medicine appropriately, attending follow-up appointments and self-management. This was extended further to highlight the importance of the relationship between the healthcare provider and the patient and, therefore, a merged definition came to light:
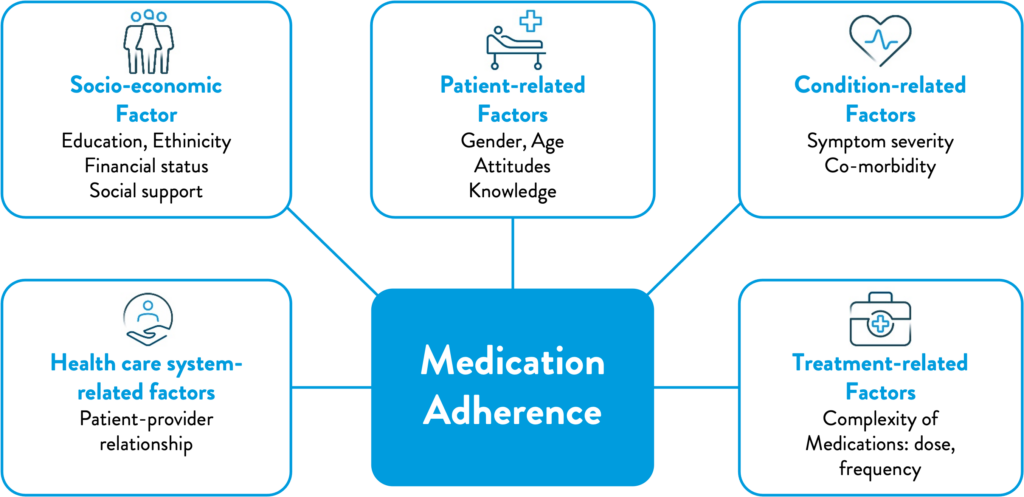
Figure 1: WHO multidimensional adherence model2
“the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a healthcare provider”.2
There are multiple stages and types of adherence
In order to gain a better understanding of adherence and patient behaviors, there needs to be a clear differentiation between intentional and unintentional behaviors. Intentional nonadherence relies on the active decision of a patient to forego a prescribed therapy. This can take place early on in the process with the non-fulfillment of a new prescription (around 15% of patients), or discontinuation of a medication without consultation from a healthcare provider (50% of patients).Conversely, unintentional non-adherence is a passive process, where patients fail to follow prescribing instructions through forgetfulness or circumstances beyond their control; it is estimated to account for 20–50% of patients.1 However, there is no clear line between intentional and unintentional non-adherence. Gadkari et al suggested unintentional non-adherence can be influenced by beliefs about medication, presence of chronic disease, and socio-demographics, which have the potential to influence future intentional non-adherence.1 With this in mind, it is important to note that adherence is not a single behavior and it encompasses a multitude of stages, including:3
- Initiation (Fulfillment): when the patient takes the first dose of a prescribed medication. The definition of this has evolved to account for being a time-to-event variable,3 corresponding from filling the prescription to the point where the first dose has been taken.
- Implementation (Compliance): the extent to what the patient is actually doing corresponding to the prescribed medication, from initiation until the last dose is completed. This can include aspects such as the proportion of prescribed drugs taken from the prescriptions; proportion of doses taken as recommended by the healthcare provider; number of drug holidays and intervals between doses.3
- Persistence: the length of time between initiation and the last dose which immediately precedes discontinuation.3
Adherence is a multifaceted behavior
Khan et al stated that the interaction between patients and their healthcare provider has a fundamental role in adherence to treatment regimens. Adherence, as a behavior, extends beyond the patient agreeing to a treatment plan. Those with chronic health conditions are more likely to demonstrate good adherence if they have an active role in the formulation of their treatment plans.4 Shared decision-making allows for patients and healthcare providers to be equal in developing and monitoring their care. Not only does this build trust, but it ensures that expectations and therapy goals are aligned with the healthcare provider and the overall role of the treatment within the patients’ lives.
Systemic factors in adherence/non-adherence
There are three broad reasons behind low adherence rates to chronic disease medication, encompassing many factors. There is poor awareness of the issue among all stakeholders, with health professionals underestimating the problem in their patients, and a lack of evidence supporting cost effective interventions to improve adherence. Secondly, incorrect targets for interventions and poor incentives; discussions often attribute the problem to the individual patient, rather than the elements of the health system (such as medication costs and difficulty filling prescriptions) that may be driving non-adherence. Thirdly, a lack of patient involvement in the decisions about their therapy, resulting in lack of motivation or rejection of the therapy.4
Sabate et al. stated that, globally, patients with cardiovascular disease show a pattern similar to other chronic pathologies, where there is 50% adherence in high-income countries, and the rate is even lower in low- to middle-income countries.2 These differences have been attributed to variance in geography, culture and commerce, and health resources and availability of healthcare. Poor adherence creates a vicious cycle within poorer regions where limited resources may not be utilized in an effective way.2
It is estimated that a lack of adherence accounts for 200,000 avoidable deaths in Europe each year.4 Patients who were nonadherent to statins had total healthcare cost on average of $900 more than adherent patients; and have an increased likelihood of hospitalization.5 Conversely, adherence to statins shows lower overall healthcare costs. Although medication costs might increase in the short term, this is offset by lower medical costs. In the US, improving patient adherence translates to $3 billion a year saving.6
Understanding and improving adherence to treatment
Early models relied on simple, written interventions to improve adherence, however, this was only effective in the short term. This later developed to educating patients about their disease and medication with follow up to improve adherence in the long term.7 However, as technology has progressed, the gold standard has evolved to measure patient adherence using electronic or digital devices, which enable personalized intervention if non-adherent or encourage behavior if adherent. This level of assessment allows for a collaboration between patient and healthcare provider.8
Due to the complex nature of adherence-related behaviors, it is important to develop a model that will allow for the use of effective behavioral interventions. With the development of evidence-based behavioral-intervention models, it is more likely that those interventions will have a greater effect than those based on observation alone. This does not exclude interventions based on other factors such as regimen complexity and cost of medication.7 Developing models that encompass different populations, all contributing factors, and consider different elements of the patient journey, will be an important element to improving outcomes in cardiovascular disease through improving medication adherence. These models should leverage evolving evidence and emerging technology to ensure responsibility is shared between healthcare provider and patient. The next articles in this series provide an up to date overview of the explanations for non-adherence, the interventional strategies which can used to improve adherence (articles 5 and 6) and the role of digital approaches for achieving this.
References
- Gadkari et al. Unintentional non-adherence to chronic prescriptions: How unintentional is it really? BMC Health Research; 2012; 12:98
- World health organisation (WHO) 2003 ADHERENCE TO LONG TERM THERAPIES- Evidence for Action. Available at: https://apps.who.int/iris/handle/10665/42682. Accessed December 2020.
- Vrijens et al. A new taxonomy for describing and defining adherence to medications Brit. J Clin Pharm 2012; 73:5: 691-705
- Khan et al. Investing in medication adherence improves outcomes and health system efficiency: Adherence to medicines for diabetes, hypertension and hyperlipidaemia OECD working papers; 105
- Bansilal et al. Assessing the Impact of Medication Adherence on Long-Term Cardiovascular Outcomes. J Am Coll Cardiol 2016;68(8):789-801
- Pittman et al. Adherence to Statins, Subsequent Healthcare Costs, and Cardiovascular Hospitalizations. American Journal of Cardiology 2011;107(11):1662-1666
- Holmes et al. Predicting adherence to medications using health psychology theories: a systematic review of 20 years of empirical research Elsevier 2014; 17: 863-876
- Von Heuckelum et al. The effect of electronic monitoring feedback on medication adherence and clinical outcomes: A systematic review. PLoS ONE; 12;10: e0185-453
