Methods of behavior change in medication non-adherence
- Medication adherence is a complex human behavior and a myriad of factors influence it.
- Adherence behavior is predicted and explained by different behavioral models and theories that form the basis of different behavior change methods1.
- Behavior change techniques can be targeted at an individual, organization, community, or population.
- Successful interventions are those that target several levels such as the behavior change wheel and the COM-B framework2.
Behavior is defined as the action or set of activities in response to an internal or external stimulus2. Behavior is a key risk factor for individual and public health in multiple ways. It impacts disease prevention, seeking medical attention, adhering to the prescribed treatment, and also delivery of healthcare for several diseases and also for treatment adherence. Behavior towards treatment adherence is dynamic and is prone to change as per an individual’s experiences or interaction with other behavioral patterns2.
Influencing behavior for optimal medication adherence is the “holy grail” for medication management and can turn the tide towards improved clinical outcomes. However, it has remained elusive even with a multitude of behavior change techniques being employed1. A comprehensive hierarchical taxonomy of the various techniques being employed has been documented by Michie et al, 2013. Most of these techniques are based on different theories of behavioral change discussed in the following section3.
The theories behind changing behavior
There are multiple psychosocial models to understand the contours of human health behavior. These theories help in the design of behavioral change interventions by understanding human health behavior, directing research in that area, and adapting the interventions for different health contexts and geographies1. Medication adherence is related to six major theoretical views described below. Most of the behavior change models belong to one of the following perspectives1:
1. Biomedical perspective:
This incorporates biomedical theories assuming patients to be passive recipients of doctor’s instructions. It focuses on identifying the actual biological cause of the disease and the treatment prescribed for it. Non-adherence is thought to be caused by patient characteristics like age and gender. Interventions like medication event monitoring system (MEMS) is sometimes based on this perspective1.
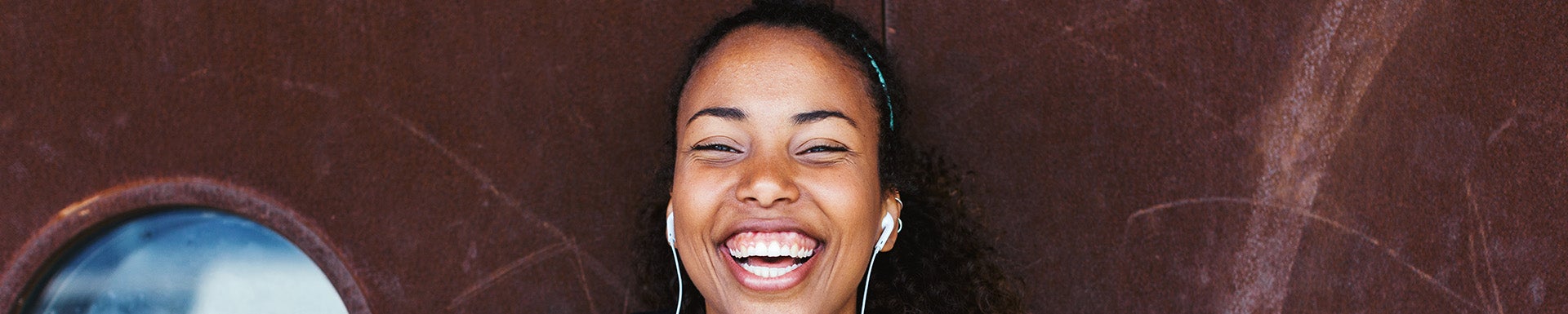
2. Behavioral perspective:
This incorporates behavioral learning theories (BLT) focused on teaching the skills for health management. It uses principles of antecedents and consequences to influence behavior. Antecedents could be internal or external and the consequences could be reward or punishment. Strategies like patient reminders are based on this perspective and are often used for medication adherence to therapy for chronic diseases1.
3. Communication perspective:
Communication between patients and healthcare practitioners is pivotal in adherence. This perspective stresses on clear comprehensive communication by healthcare practitioners and patient education. Several interventions use this communication element between the provider and the patient to enhance adherence1.
4. Cognitive perspective:
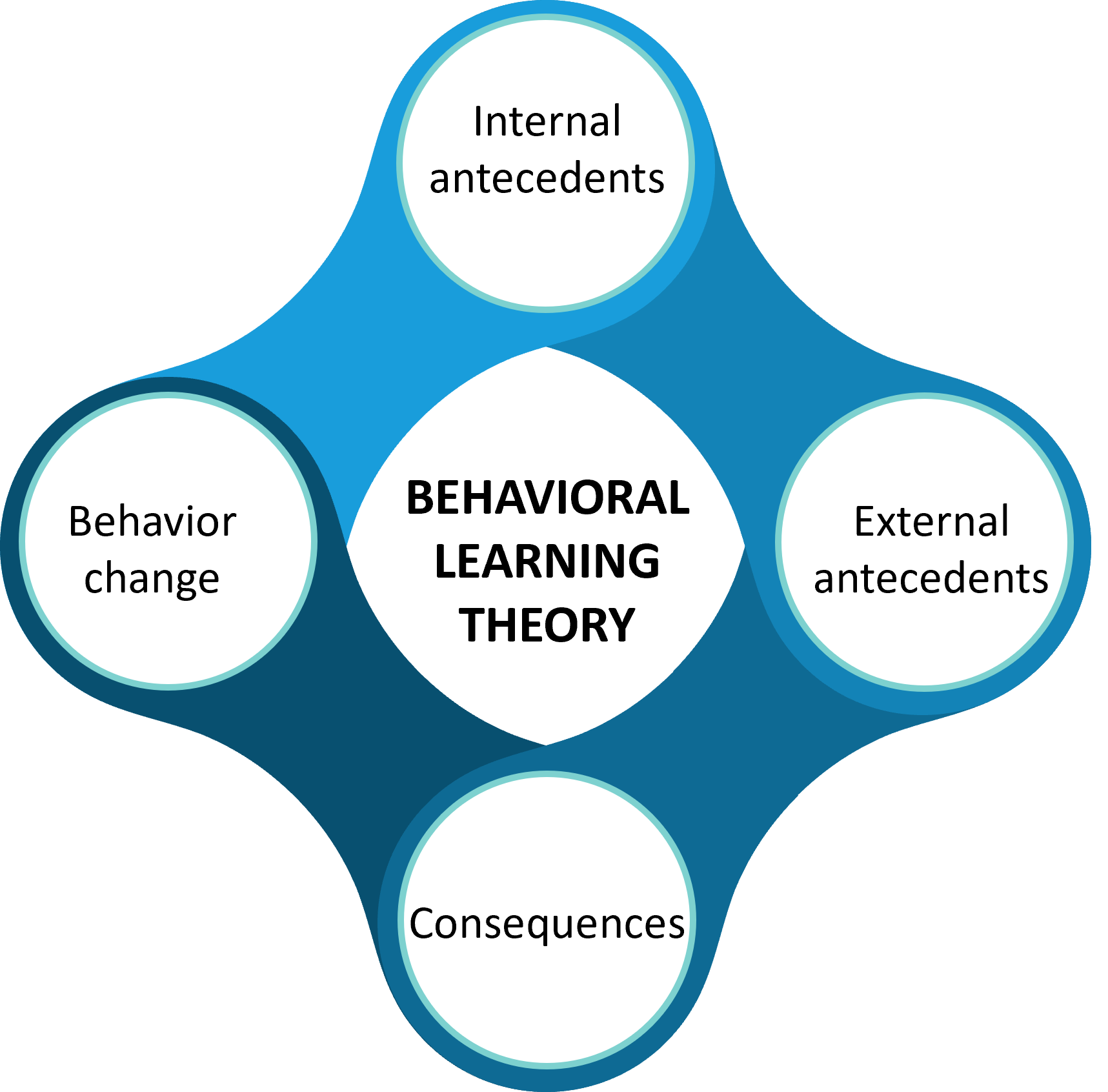
This includes cognitive behavioral theories like the health belief model (HBM), social cognitive theory (SCT), theory of planned behavior (TBP), and protection motivation theory (PMT) (discussed below in detail). These theories take into account patients’ cognitive aspects as key factors for behavioral change. They imply that patients’ attitudes, beliefs, and expectations about the outcome as the major determinant of health behavior1.
- The Health belief model: The model is rooted in the rational viewpoint of threat perception, barriers to behavior, and benefits of action. The two founding principles for health-related behavior are 1) the desire to get well or prevent disease and 2) belief in certain health actions to cure or prevent disease. Ultimately, the action depends upon a person’s perception of the benefits counterbalanced by various barriers to health behavior1,4. HBT has been used in understanding adherence to practices for COVID-19 prevention5. The six constructs of HBM that influence behavior are the following:
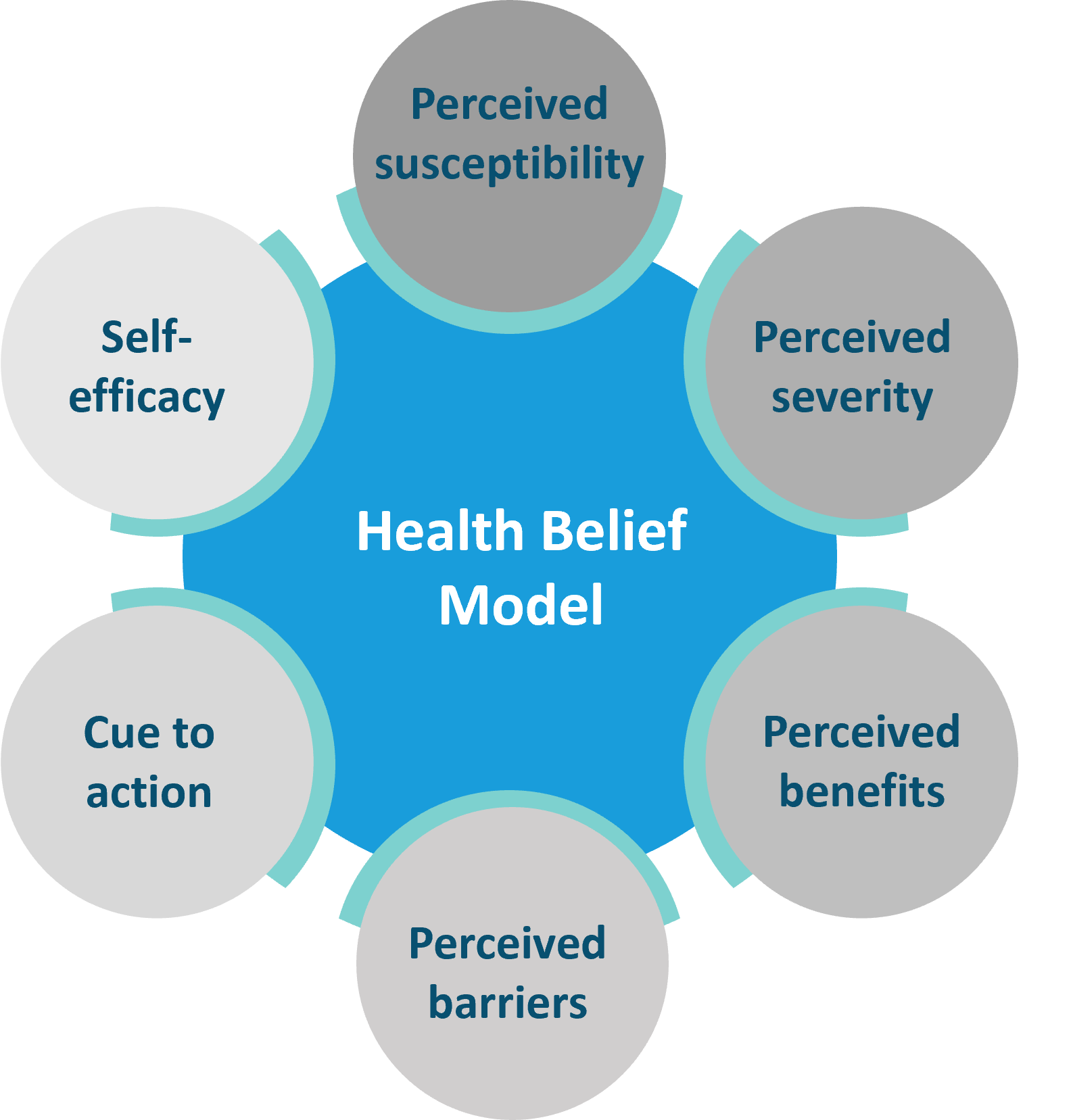
- Social cognitive theory: The model stresses the importance of social context on an individual’s behavior. There is a dynamic and reciprocal interaction between the person and the environment that shapes behavior. Adhering to medical treatment is a behavior influenced by both personal and environmental factors1,4. Recently, a study evaluated adherence to breast cancer therapy using the SCT model and found that although the medication-taking action is a deeply personal behavior, it is simultaneously influenced by several external factors6. SCT also aids in reinforcing health behavior and therefore in its maintenance. The six constructs of SCT that influence behavior is the following:
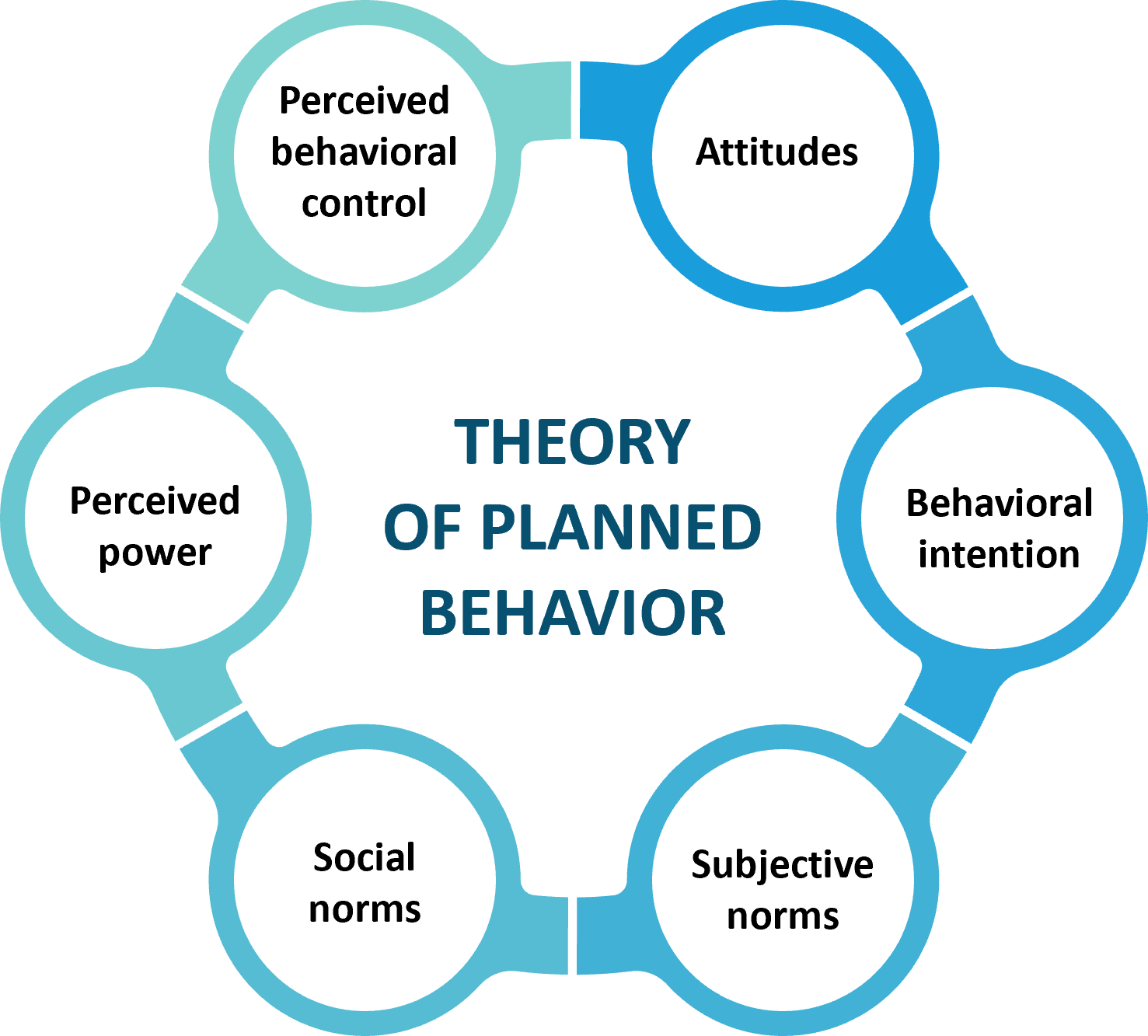
- The theory of planned behavior: The theory of planned behavior or reasoned action predicts an individual’s intention to engage in a particular health behavior. The key component of this model is the individual’s intent influenced by the attitude emanating from belief about the expected outcome and evaluation of risks and benefits of the outcome. Finally, the behavior is achieved through motivation (intention) and ability (behavioral control) 1,4. The six constructs of TPB that influence behavior are the following:
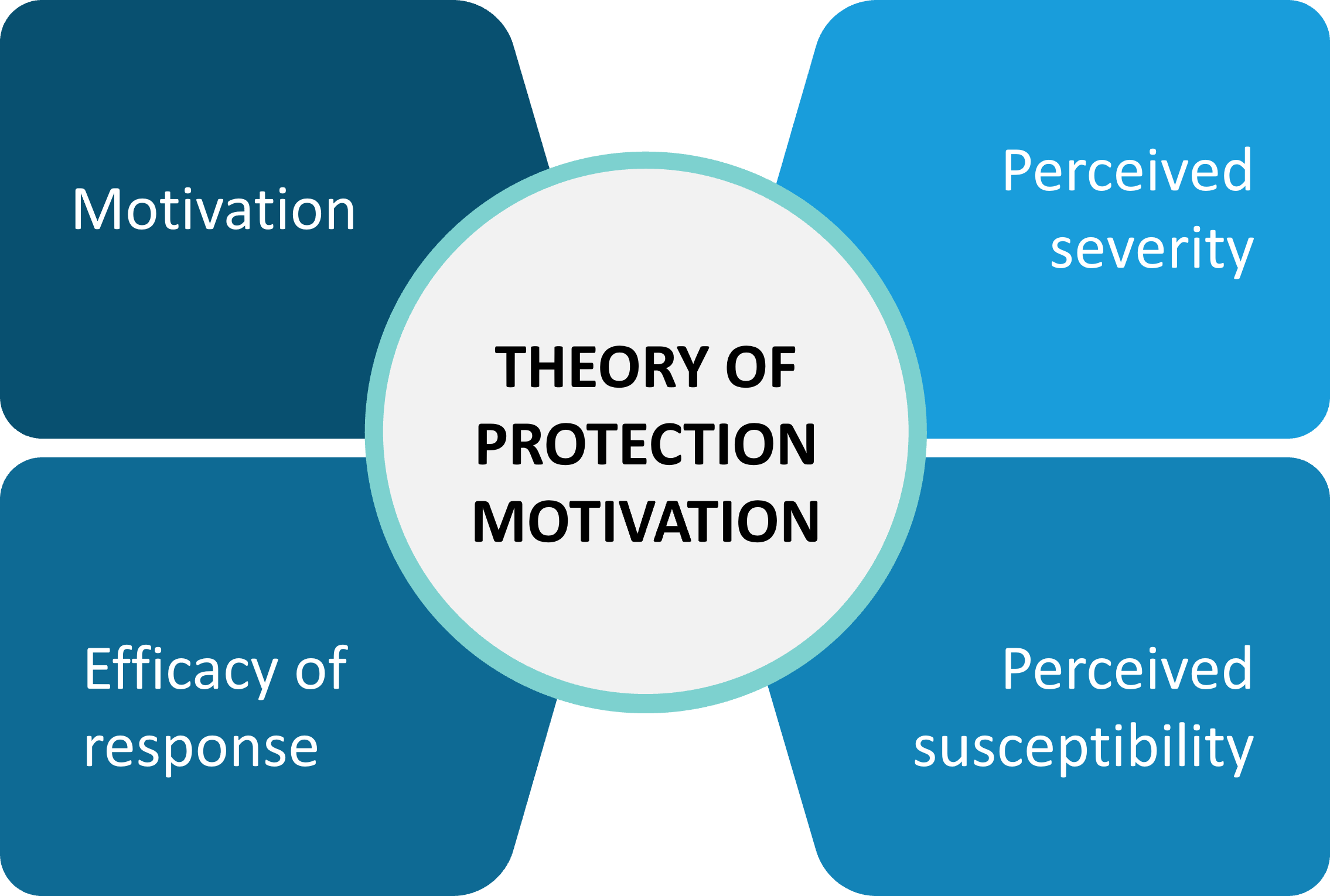
- Theory of protection motivation: This model dwells on understanding human behavior in response to a threat and the factors that motivate behavioral change in such situations. It tries to predict and explain the decision-making process and coping strategies in the event of a perceived threat to protect oneself. Therefore, threat appraisal and coping appraisal are two main components of this theory1.
- Limitations of cognitive behavior theories: Cognitive behavioral theories try to predict and explain human health behavior based on the cognitive perspective and posit that individuals will make choices based on expectations of a positive outcome. However, it doesn’t take into account the non-voluntary factors that could influence behavior. Also, these theories do not necessarily address the behavioral skills that are required for medication adherence. The root cause of various beliefs and the origin of patients’ attitudes towards medication are also not incorporated in these models. They also focus on just one threat and prevention behavior, often ignoring other threat perceptions that might influence the medication-taking behavior1.
5. Self-regulatory perspective:
This includes a focus on an individual’s subjective experience to health threats and their response towards it. The self-regulatory theory is the main model in this domain1.
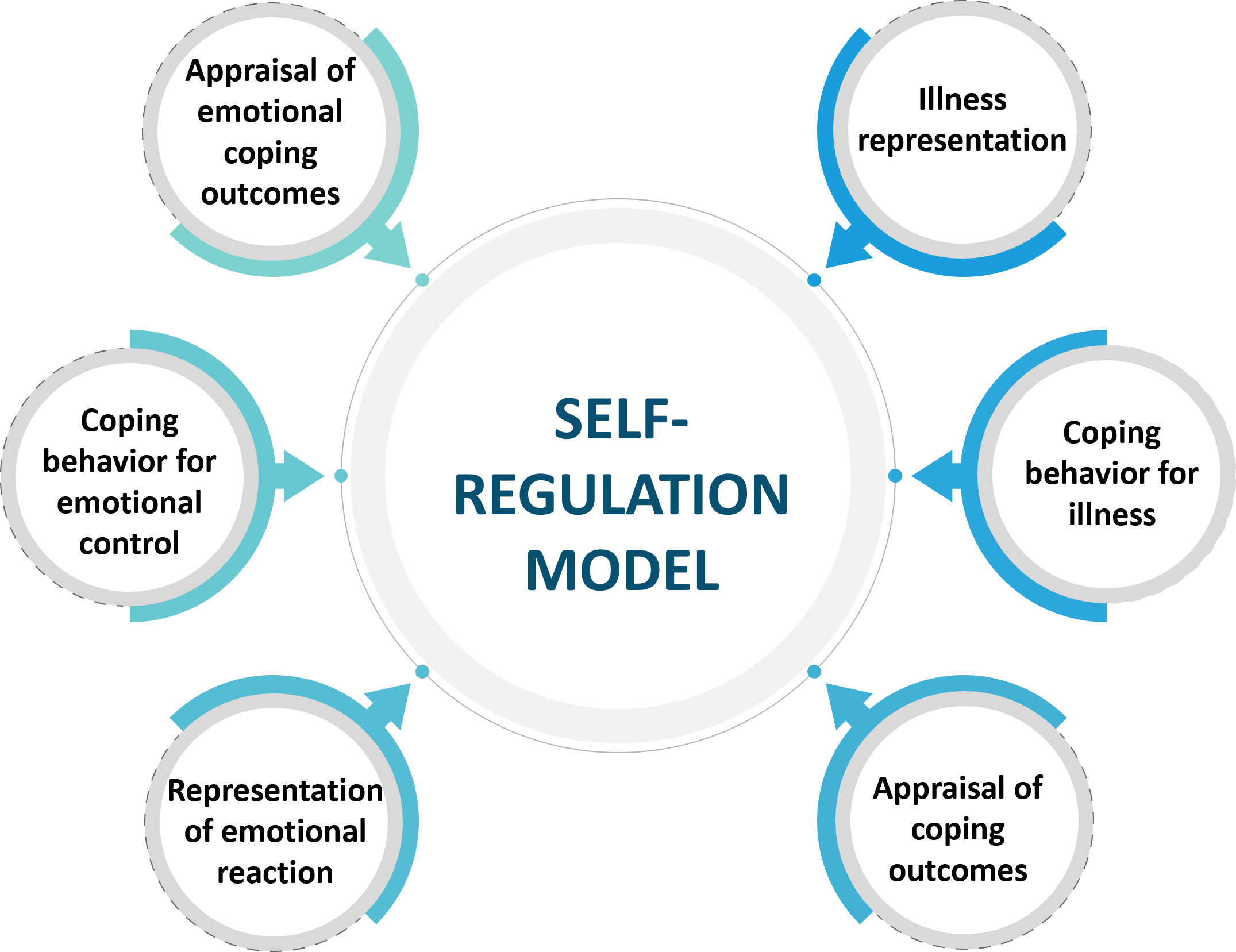
- Self-regulation model: This model posits that Individuals form cognitive representation of health threats based on past experience and also take into account new information. These guide their choice of coping strategy. The model focuses on the way individuals select their goals for daily activities and choose behaviors to complete them and has following components1,7:
6. Stage perspective:
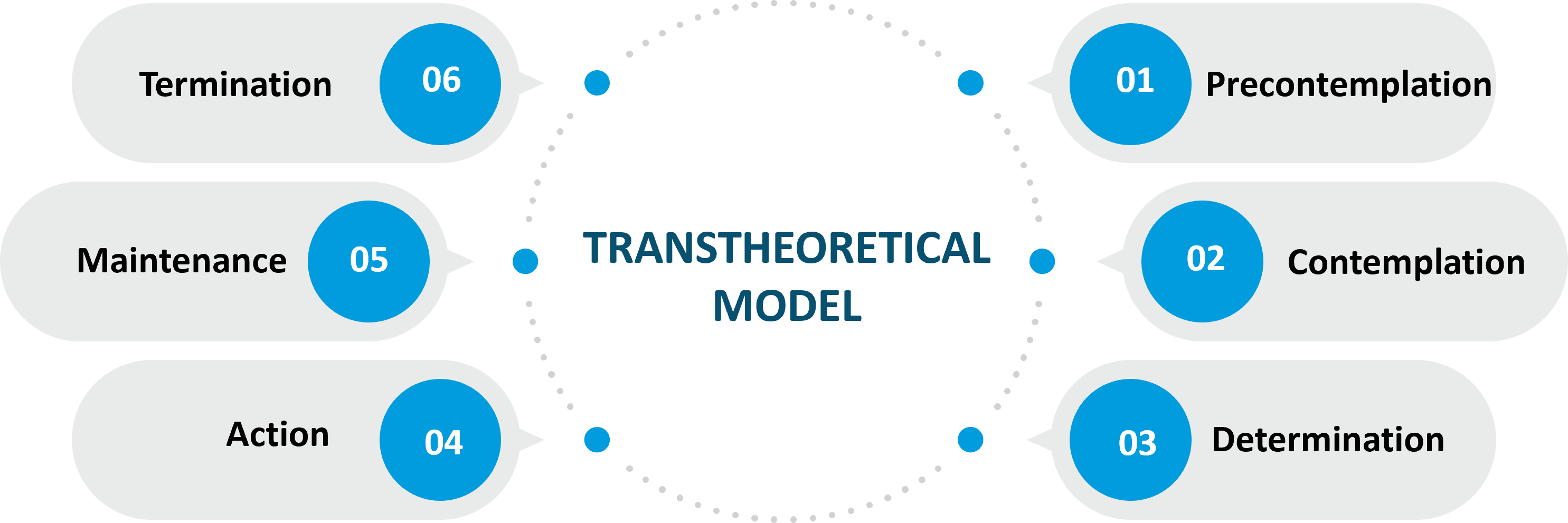
This perspective highlights the presence of multiple qualitative discrete stages in the process of behavioral change. While moving through these stages, individuals can relapse to the previous stage. The theory of the transtheoretical model (TTM) addresses this perspective1.
- The trans-theoretical model: This is a model which focuses on understanding the process of behavioral change. The model posits that behavior change is a slow process that doesn’t happen decisively at one time, but continuously often in a cyclical manner. It proposed the following six stages of behavior change1,4.
Behavior change techniques:
It is a challenging task to design behavioral interventions based on these health behavior theories and adapt them to address medication non-adherence1. Some commonly used behavioral change techniques are described below.
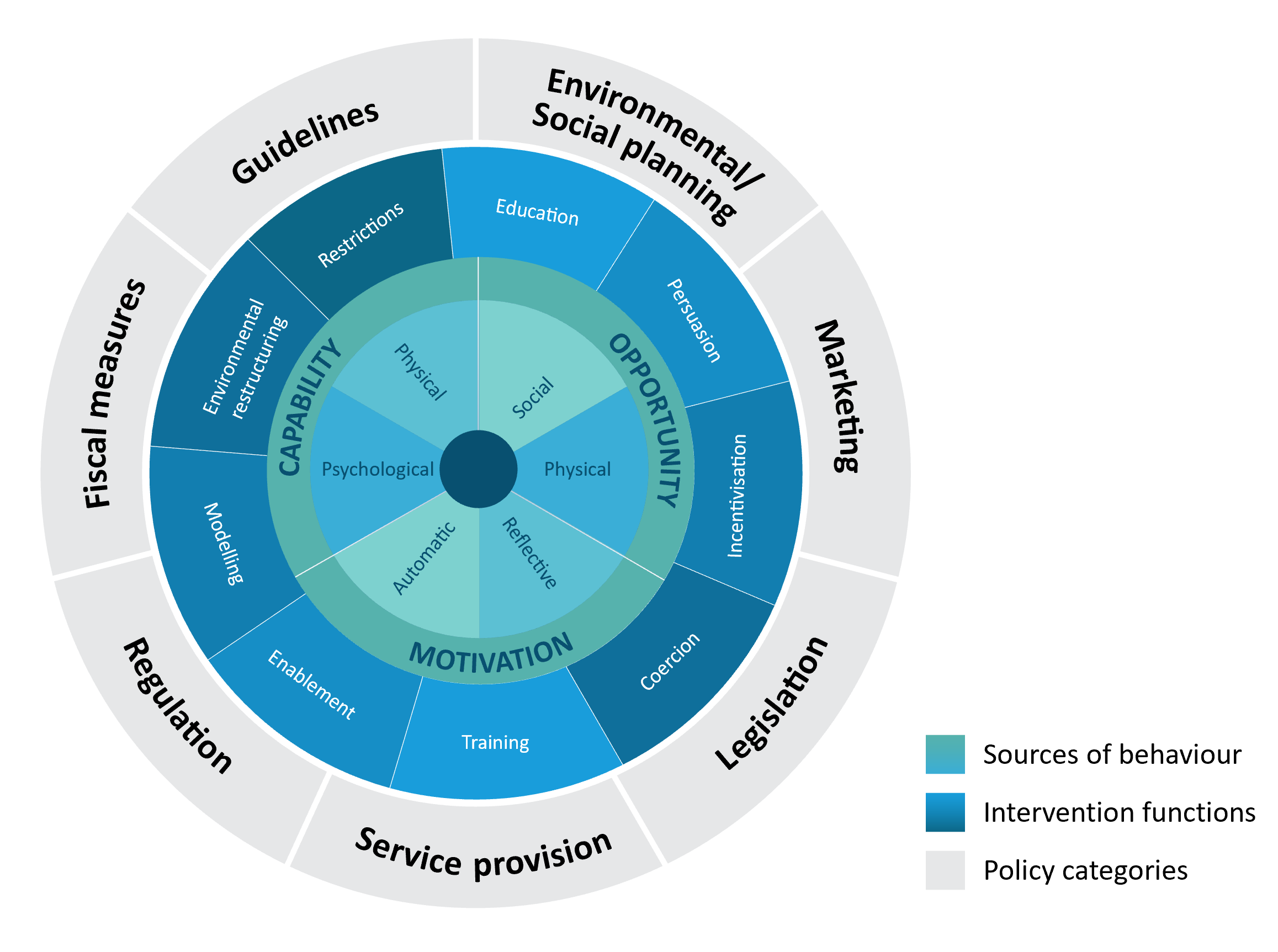
- COM-B model: As per NICE (National Institute for health and care excellence) 2014 recommendations, interventions aimed to change individual behavior should focus on:1) goals and planning, 2) feedback and monitoring, and 3) social support. COM-B (Capability, Opportunity, Motivation, Behavior) model encompasses these recommendations to influence behavioral change. Capability refers to an individual’s physical ability for change, opportunity refers to the social or external environment receptive to change, and motivation refers to intent or belief in change2. For more on this, see our article: The COM-B framework and its use in explaining non-adherence.
- Nudge theory: It is described as any aspect of choice architecture that can cause a change in behavior without forbidding any options or giving significant economic incentives. Typically it includes restructuring the environment, modeling, and non-economic incentivization2. For more on this, see our article: “Nudging” patients towards better adherence to improve outcomes.
- The behavior change wheel: It is a comprehensive framework based on 19 different behavior change techniques. It provides a systematic guide for designing behavior change interventions. It has COM-B model at its core surrounded by two concentric layers of intervention strategies. The first layer of the ring describes nine direct methods of behavior change while the outermost layer of the ring deals with the policies or strategies to be applied at the societal or institutional level for implementing and sustaining behavior change2.
For more on behaviour change wheel, see our article: The Behavior Change Wheel: A framework for improving menopause therapy adherence.
- Motivational Interviewing: It is a patient-centered approach to explore the patient-specific barriers for non-adherence and elicit a change in their behavior in an atmosphere of acceptance, trust, and compassion8.The key factors in designing MI are:
- Not imposing change on patients
- Starting a conversation about non-adherence and reflective listening
- Helping resolve the ambivalence by motivating a change in will
- Being patient through the change in behavior, which is often a variable timeline than a fixed timepoint
For more on this see our Session: Improving medication adherence with motivational interviewing – example of a heart failure patient
Future Directions:
Currently, the key challenge is to assess the usefulness and efficacy of various behavior change interventions. The Human Behavior-change Project is striving to address this issue through a multidisciplinary team of experts ranging from behavior scientists, to computer scientists, and information scientists. The goal of this project is to aid in an improved understanding of human behavior and identification of effective methods to bring-out change in behavior2.
“The most important thing in changing human behavior is the person’s motivation” – Milton H Erickson, American Psychiatrist.