Supporting adherence: Leveraging the power of family and peers
- Family and peers are key pillars of social support, playing a critical role in improving medication adherence.1
- They provide both emotional and practical support, enhancing patients’ self-efficacy and encouraging positive behavior change.2
- Healthcare providers can leverage this support by evaluating a patient’s social support and by implementing targeted family- and peer-based interventions.3
Chronic diseases are the leading cause of death and disability across the world.1,4 The management of chronic diseases predominantly occurs outside hospital settings and requires long-term therapeutic interventions.5 The epidemiological shift from acute to chronic diseases has rendered the model for the acute care health service delivery inadequate to address the challenge of chronic care.1 The success of chronic disease treatment greatly depends on patients’ adherence to treatment.6
According to the World Health Organization (WHO), adherence to long-term therapies is simultaneously influenced by factors such as disease characteristics, healthcare, socio-economic, therapy- and patient-related factors. To care effectively for chronic conditions, WHO posits an important role for family and community members, which is necessary to affect health outcomes and behaviors.1
Adherence is a behavior: Family and peers can influence behavior change
Medication adherence is a dynamic process,1 and non-adherence is a variable behavior that varies between patients and within patients.7 Learn more about Behaviors and beliefs: the foundations of adherence in the a:care Congress session by Rob Horne, Professor of Behavioral Medicine, University College London, UK.
Improving adherence is a continuous process requiring follow-up throughout the treatment course.1 As explained by John Weinman (Professor of Psychology as applied to Medicines, King’s College London, UK) in the masterclass on Behavioral frameworks for understanding patient adherence, interventions such as provision of information and medication reminders only work in the early phases of adherence. Sustained adherence requires behavior change. A person’s behavior is strongly dependent on their beliefs, which are shaped by the family and community in which they live. As per the Capability, Opportunity, Motivation–Behavior (COM-B) model of behavior change, family and peer support are integral to the patient’s behavior change journey. To understand more about how beliefs impact medication adherence, read our article Impact of belief and misconception in medication non-adherence.
Sustained adherence often depends on strong family involvement and social support, which are crucial in encouraging optimism and self-esteem, reducing stress, and giving practical assistance.8
Family and peer support: Key to adherence in vulnerable patient populations.
Although most chronic disease patients require supportive and positive social interactions, certain groups are particularly vulnerable and depend on their family and friends for managing health conditions, such as:
- Young children: Young children are often poorly adherent to their treatment, and it is largely dependent on the ability of parents and guardians to follow through with the recommended treatment.1 Family support was found to be associated with fewer adherence barriers and greater intent to adhere in the pediatric population.9
- Adolescents: Sustained parental involvement with minimizing conflict encourages treatment adherence in adolescents.1 For more on this, please read our article Medication adherence in adolescents – challenges and interventions. It has been proposed that their underlying belief system is largely influenced by the core beliefs of the family or community in which they live.9 In a study on adolescents and preadolescents with cystic fibrosis, parental supervision was associated with better adherence to treatment.10
- Elderly: They have complex health needs and may simultaneously suffer from physical and cognitive decline, making medication adherence challenging.1 Family plays a key role in medication management activities of older patients such as assisting with administering medications, conveying medical information and receiving feedback, as well as participating in decision making.11
- Mental health patients: Patients with mental health issues are particularly vulnerable to non-adherence.1 As discussed in our articles, Non-adherence in patients with schizophrenia: An issue of impaired insight and Medication compliance in mental health for improved treatment outcome, mental health patients lack insight and understanding of their health condition, and suffer from disease-related stigma that impacts treatment adherence. A family-focused therapy that includes family members in the treatment plan, including family psychoeducation, is shown to reduce relapse rates and facilitate recovery.12
How can family and peers support medication adherence?
Family and peers can benefit patients by providing emotional and practical support, reducing stress, increasing self-efficacy, and influencing behavior change. The odds of adherence to treatment in patients living with their spouse was found to be 1.27 times higher than unmarried patients. It is reported that cohabiting with other adults – not just spouses – has a positive influence on adherence behavior (P<0.05). Additionally, the quality of a family-patient relationship is more important than the mere presence of a family member. The odds of adherence are three times higher in cohesive families that display warm, accepting, and closer relationships as compared to non-cohesive families. A meta-analysis of 122 studies found medication adherence to be 27% higher in patients when they had practical support available.2
Peers can help in addressing the psychosocial isolation experienced by patients suffering from chronic stigmatized diseases such as HIV/AIDS. Peer or buddy programs capitalize on patients’ ability to relate to a peer as both have common needs and concerns. They can be each other’s role model as well as provide a resource for coping techniques and experiential knowledge. Peers act as sounding boards for things that could be burdensome for the family, help in normalizing the required behavioral changes, and provide low-key behavioral monitoring.13
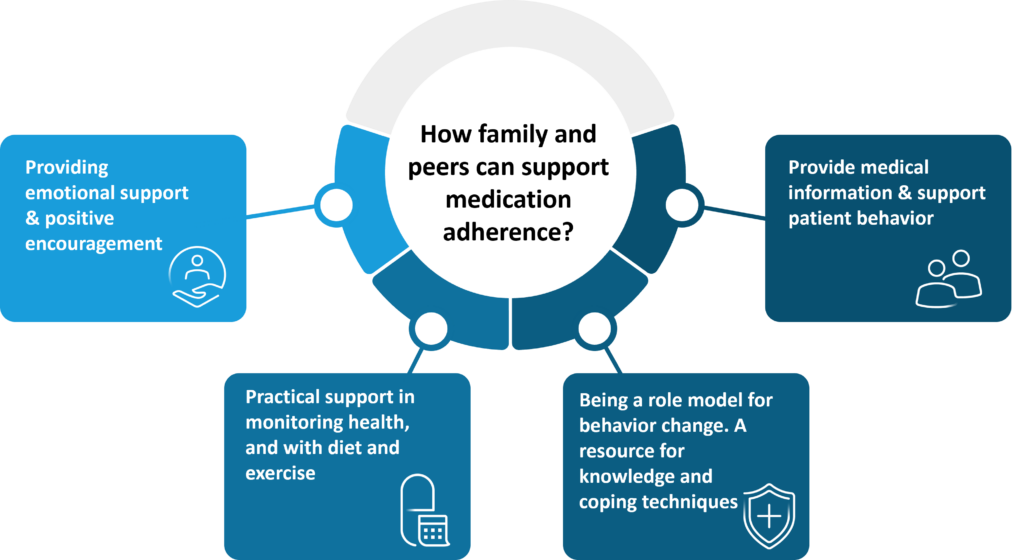
Figure 1: Role of family and peer support in medication adherence.
(The image is only for illustration purposes and the content is from Miller et al. 2013, Shahin et al., 2007 and Marino et al., 2007.2,3,13)
Harnessing family and peer support: A guide for healthcare providers to improve adherence
- Behavioral family systems therapy: A family-focused, multifaceted approach enhancing communication between family, problem-solving skills, improving family beliefs, cognitive restructuring, and functional-structural family therapy. This intervention is shown to improve adherence to diabetes treatment, metabolic control in adolescents, and reduce family conflicts.2
- Family health and psychoeducation: Patient health education is widely used to improve medication compliance across a broad range of chronic illnesses and is considered integral to disease management programs.1 Involving family members in patient education can reduce symptoms and relapse rates in patients with mental health issues like schizophrenia.12 Similarly, in a study, self-management education in parents of asthmatic patients resulted in reduced emergency department visits.1
- Peer support program: Peer support programs are supportive communities designed to offer informational and psychosocial support to patients and reduce their social isolation. These programs connect patients and caregivers to others who have similar experiences with the same health condition and who can provide practical information about self-care and guidance in navigating the health system.15
- Engaging community organizations: Studies have shown that families and peers of patients are usually willing to accept messages from the community.The providers’ national and local associations and allied bodies, including public health associations, can adopt an active partnership with the community, which can increase the health knowledge base of community members.14
Family and peer support in action: Successful adherence interventions
A review of studies analyzing the impact of peer-delivered interventions, where peer was defined as individuals suffering from the same chronic conditions as the target population, reported a positive impact on medication adherence. The type of interventions administered in these studies included peer telephone support, face-to-face visits, sharing disease/therapy information, peer mentoring, and group classes. The studies reported a low attrition rate for the interventions and positive changes in other health behaviors like exercise and physical activity. Notably, the highest impact on medication adherence was reported in the studies using face-to-face contact time with peers.16
Similarly, a review analyzing the role of family in improving medication adherence and quality of life (QOL) in patients with tuberculosis revealed higher adherence rates (P<0.05) in patients receiving robust family support. Additionally, the study reported enhancement in the QOL of these patients. Family members played a vital role in supervising the medicine intake by direct observation and encouraged patients, providing them confidence in the treatment plan. The family-based interventions included bi-weekly home visits that provided psychoeducation and health education focused on TB. The sessions allowed families to express their concerns and share insights on self-care practices.17
Ask your patients about social support: Quality counts for adherence
Family and social support are beneficial and improve medication adherence. However, a negative social environment that lacks support, stigmatizes disease and associated treatment, or presents competing demands is an active barrier to medication adherence. Thus, the ways in which social support can directly and indirectly affect outcomes are complicated.2 Healthcare providers need to evaluate the type and quality of social support available to the patient and assess if it can assist the patient’s treatment journey. On the other hand, patients without adequate support may need to be directed towards appropriate community resources and social workers for optimal medication adherence.3
“Recognise that the patient does not come as a ‘blank sheet’ that we can write the prescription instructions on”
– Rob Horne, Professor of Behavioral Medicine, University College London, UK













