How to Improve Diabetes Medication Adherence: A Guide for Healthcare Professionals
Medication adherence in type 2 diabetes is a widespread challenge, especially in resource-limited settings. Many patients struggle to take medications consistently, which leads to suboptimal glycemic control and preventable complications. 1
Studies show that roughly half of patients do not take chronic disease medications as prescribed, and poor adherence is linked to higher hospitalization rates and even mortality in diabetes.2
As healthcare professionals, understanding why adherence falters and how to improve it is key to better patient outcomes. In this guide, we answer common questions primary care providers ask about improving medication adherence in type 2 diabetes, offering practical tips grounded in behavioral science (including the COM-B model) and supported by medical evidence.
Why is it so important for my patients to stick to their diabetes medications?
Sticking to diabetes medications is critical because missing doses leads to higher blood sugar levels, more complications, and worse health outcomes. Patients who do not take medications as prescribed often fail to achieve glycemic targets. At least 45% of people with type 2 diabetes have HbA1c above goal, partly due to poor adherence.1 Non-adherence has been associated with disease progression and increased risk of complications like heart and kidney disease.3 In fact, in US poor medication adherence is estimated to account for up to 69% of medication-related hospital admissions and tens of thousands of deaths each year.4 On the positive side, when patients take their medications regularly, they tend to have better blood glucose control, fewer diabetes-related emergencies, and improved quality of life.5 In short, emphasizing adherence is not just about “taking pills”. It’s about preventing serious complications and saving lives.
Why do many patients struggle to take their diabetes medication as prescribed?
Many patients struggle with adherence due to a mix of practical, psychological, and social barriers. Common reasons include the cost of medications, complex or lengthy treatment regimens, side effects, and simple forgetfulness.1 Socio-cultural factors and health beliefs also play a role. For example, some patients may be in denial about their diabetes or lack understanding of why the medication is needed, leading them to skip doses. Fear is another barrier: patients might fear side effects or insulin injections, or feel overwhelmed by having a chronic disease.1,6 Low health literacy and language barriers can prevent patients from understanding instructions, resulting in misuse or non-use of medications6. Additionally, external challenges like unreliable access to pharmacies, long travel distances, or running out of medication can lead to gaps in therapy.7 In essence, non-adherence is usually multi-factorial. It’s rarely just “patient forgetfulness,” but often a combination of knowledge gaps, attitudinal barriers, and logistical difficulties.8 Recognizing these root causes is the first step in helping patients overcome them.
How can I help my patients remember to take their diabetes medications on time every day?
Healthcare professionals can help patients build habits and use tools to remember their medications. The first step is simplifying the regimen whenever possible, for instance, switching to once-daily dosing or fixed-dose combination pills can dramatically reduce the chance of missed doses.1,9 With a simpler schedule, patients have fewer things to remember. Next, encourage the use of practical reminders: recommend pill organizers10 (weekly pill boxes) so they can pre-sort doses, or suggest setting alarms on their phone for medication times. Many patients find it helpful to tie medication intake to daily routines (like taking pills right after breakfast or before brushing teeth at night), which turns it into a habit. For tech-savvy patients, there are mobile apps and text message reminder services that prompt them to take medications, even simple SMS can improve adherence in diabetes.11 Regular follow-up contact is another powerful tool: studies show that frequent check-ins by phone or text from healthcare providers can significantly boost medication adherence and improve glycemic control.12 Some tangible tips you can share with patients include:
- Use a Pill Organizer: Filling a weekly pill box can prevent missed doses by providing a visual cue and making it obvious if a dose was skipped.13
- Set Daily Alarms: Encourage patients to set phone alarms or calendar alerts for when each dose is due. Pairing medication times with daily events (meals, bedtime) also reinforces the routine.14
- Leverage Family Support: If appropriate, involve a family member to help remind or check in on the patient’s medication schedule (especially for elderly patients).14
- Simplify the Schedule: Work with the patient to eliminate unnecessary complexity – for example, once-daily or twice-daily regimens are easier to remember than medications taken multiple times a day. If multiple drugs are needed, consider combination pills or coordinating dosing times together.9,14
- Plan for Refills: Advise patients to mark refill dates on a calendar or use pharmacy auto-refill services so they don’t run out of medication.15 Where available, 90-day supplies of chronic medications can reduce pharmacy trips and help continuous supply.16
By proactively introducing these memory aids and simplification strategies, you can help patients turn medication-taking into a consistent part of their daily life.
How can I address my patients’ fears and misconceptions about diabetes medications?
Addressing patient fears and misconceptions starts with open, non-judgmental communication and good education. Invite patients to share any concerns or beliefs about their medications. Patients often worry about side effects, dependency, or have heard myths (for example, a misconception is “if I start taking drugs for diabetes, I would need to take it for life. So I had better not start taking it”).17,18 To tackle these issues, create a safe space for discussion: reassure patients that it’s common to have concerns and that you’re there to help, not scold. Ask open-ended questions in a compassionate way (e.g., “Many people experience side effects or have difficulty with medications. What worries or discomfort have you had?”). This approach helps patients feel heard and more willing to reveal barriers.
More information: Strategies to develop a therapeutic alliance for medication adherence https://acarepro.abbott.com/articles/general-topics/therapeutic-alliance-in-medication-adherence/
Once concerns are on the table, provide clear, tailored education to dispel any myths. Explain how the medication works and the consequences of not treating diabetes (e.g. untreated diabetes can silently damage organs even if one feels okay today). Emphasize the proven benefits: for instance, remind them that their medication can prevent serious complications and help them feel healthier in the long run. If fear of side effects is an issue, acknowledge it and discuss ways to manage or monitor side effects. Knowing that you will help them handle any adverse effects can reduce anxiety. It’s also helpful to share success stories or examples of other patients who overcame similar worries and saw improvements.
Building trust is crucial: patients are more adherent when they feel their provider listens and genuinely cares.19 Use simple language (avoiding jargon) and check their understanding by asking them to repeat key points. Encourage questions. Sometimes involving family members in education (with the patient’s permission) can reinforce the message and provide additional support at home. If deep-seated beliefs or emotional barriers exist, consider behavioral techniques like motivational interviewing. This patient-centered counseling method has been shown to improve adherence by exploring ambivalence and strengthening the patient’s own motivation to take medications.20 The bottom line is to treat patients as partners: by validating their feelings and correcting misinformation with empathy, you can often turn resistance into willingness.
More information: A:care masterclass by Dr Sheri Pruitt https://acarepro.abbott.com/masterclasses/how-healthcare-providers-can-address-non-adherence/
What is the COM-B model, and how can it help improve medication adherence?
The COM-B model is a behavioral science framework that can help you systematically identify why a patient is non-adherent and how to intervene. “COM-B” stands for Capability, Opportunity, and Motivation – three essential factors that must be present for a behavior (in this case, taking medication) to occur. In practical terms, COM-B prompts you to ask: Does the patient have the capability to take the medicine? Do they have the opportunity to do so? And are they motivated to stick with it?21
More information about the COM-B model: Explaining non-adherence – The Capability, Opportunity, Motivation, and Behavior (COM-B) framework https://acarepro.abbott.com/articles/cardio-metabolic/capability-opportunity-motivation-behavior-framework/
Often, adherence problems can be mapped to one or more of these areas:
- Capability: This includes the patient’s knowledge and skills, as well as physical ability, to follow the treatment. For example, does the patient understand their dosing schedule and have the memory capacity to manage it? If a patient keeps forgetting doses or doesn’t know why the medication is important, that’s a capability gap you can address with education or memory aids.22
- Opportunity: These are external factors that facilitate or hinder taking medication. Opportunity can be physical (having access to the medication, ability to afford it, a safe place to store it) and social (support from family, a routine that prompts medication use, cultural acceptance).21 For instance, if a patient cannot regularly get to the pharmacy (transportation issues or clinic far away) or struggles to pay for refills, their opportunity is limited. Likewise, lack of family support or a chaotic home environment can make adherence much harder. Identifying opportunity barriers allows you to intervene, perhaps by arranging mail-order refills, connecting the patient with financial assistance, or enlisting family members to help.
- Motivation: This covers the internal processes that drive or inhibit the behavior. Motivation can be reflective (conscious beliefs, intentions, “rational” considerations) or automatic (emotions, habits, impulses).21 A patient’s beliefs about their illness and treatment are critical here. Do they believe the medication is necessary and will help (high motivation), or do they doubt its efficacy, worry about side effects, or feel stigma about taking it (low motivation)? For example, a patient who feels “fine” when skipping pills might not see the immediate need for medication, especially if they don’t fully accept their chronic condition. Depression or fatalism can also sap motivation. To address motivational barriers, strategies like eliciting the patient’s personal health goals, correcting misconceptions (as discussed above), and providing encouragement and positive feedback can be effective. Sometimes, simplifying the regimen or reducing side effects (capability/opportunity fixes) will indirectly boost motivation because the treatment no longer seems as burdensome.
More information about the COM-B model: A:care Masterclass by Prof John Weinman https://acarepro.abbott.com/masterclasses/behavioral-frameworks-for-understanding-patient-adherence/
By using the COM-B lens, you can pinpoint why a particular patient isn’t adhering and tailor your approach accordingly.21 For instance, if capability is the issue (they keep forgetting), focus on reminders and education. If opportunity is lacking (medications are too expensive or hard to get), work on access. Maybe switch to affordable generics or monthly blister packs. If motivation is low (they aren’t convinced treatment is needed), spend time on counselling, addressing beliefs, and perhaps enlist peer support or motivational interviewing. This framework ensures that interventions target the real underlying cause rather than using a one-size-fits-all approach.
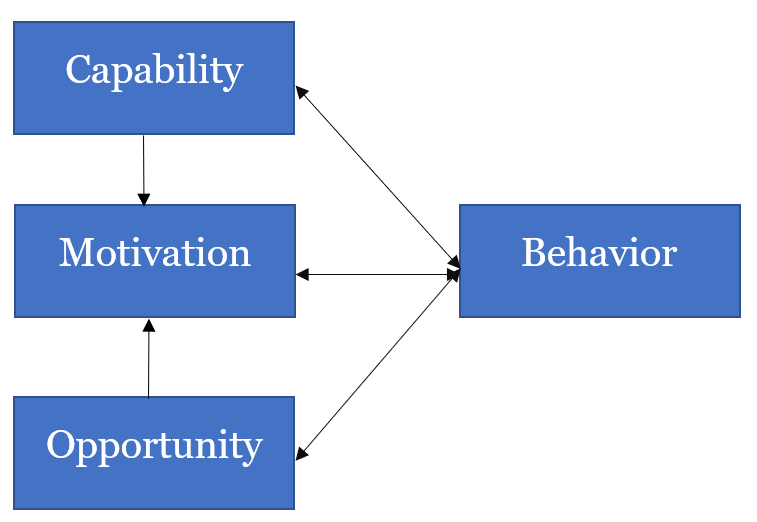
Figure: The COM-B model of behavior, illustrating that Capability, Opportunity, and Motivation all interact to drive a behavior (such as taking medication). If any component is insufficient (e.g., a patient lacks the knowledge, resources, or drive to take their medications), adherence can suffer. Using this model helps healthcare providers identify which component to strengthen for each individual patient.21
Importantly, COM-B is one of several behavioral models available. Other frameworks like the Health Belief Model https://acarepro.abbott.com/articles/cardio-metabolic/health-belief-model-examples-diabetes/ (which focuses on patients’ perceived susceptibility, benefits, and barriers) and the Transtheoretical Model (stages of change) https://acarepro.abbott.com/articles/central-nervous-system/the-transtheoretical-model-and-the-stages-of-patient-adherence/ can also offer insights into patient adherence behaviors. In practice, these models often overlap. The key takeaway is that improving adherence often requires a behavior change approach, understanding the human factors behind why patients do or don’t take their medications, and then applying targeted strategies to influence those factors.
How can I motivate my patients to take their medication and make healthy lifestyle changes?
Motivating patients for both medication adherence and lifestyle changes (like diet and exercise) requires a supportive, patient-centered approach. Start by helping patients set achievable goals and linking their medication routine with their broader health goals.23 For example, if a patient’s goal is “to avoid complications so I can provide for my family,” remind them how taking medication daily and exercising regularly will help keep them healthy to meet that goal. It’s important to emphasize that medications and lifestyle modifications go hand-in-hand. Optimal glucose control is achieved through both proper medication use and healthy lifestyle changes, which together prevent long-term complications. In other words, medication isn’t a substitute for diet/exercise, and vice versa; they reinforce each other as part of a complete diabetes management plan.24
One effective tactic is to break down changes into small, manageable steps.25 Patients can get overwhelmed if you ask for too much change at once. Instead, collaboratively choose one or two specific areas to work on. For instance, you might agree on a goal of taking medication with breakfast every day (linking it to a meal habit) and walking for 15 minutes in the evening three times a week. These small successes build confidence (self-efficacy) and momentum. Positive reinforcement is crucial: praise patients for any improvements or efforts they make, no matter how small.26 When they see progress (e.g., a slight drop in HbA1c, weight loss, or just feeling more energetic), point out that their hard work and consistency paid off. This reinforces their motivation to continue.
Regular follow-up and encouragement from the healthcare team can significantly boost a patient’s motivation.26 A quick phone call or message to check in on how they’re managing can remind them that you’re invested in their success. Patients who feel supported by their providers (and family) are more likely to stay motivated to adhere. It also helps to normalize the struggle: let them know that it’s human to slip up and that you are there to help them get back on track without judgment. If a patient is particularly resistant or ambivalent, consider more formal behavioral support: diabetes educators, nutritionists, or counselors can provide additional coaching and motivational interviewing. Some patients respond well to peer support as well, connecting them with a diabetes support group or a “buddy” who has successfully made lifestyle changes can inspire them through real-life examples.27
Finally, ensure that the patient truly understands the “why” behind both medication and lifestyle recommendations.28 Patients are more motivated when they comprehend the benefits (e.g., “Taking your medication and walking daily will likely improve your energy and protect your kidneys and heart in the long run”) and the risks of non-adherence (“If we skip these, your blood sugar may stay high and silently cause complications”). Education should be ongoing and tailored to their level of health literacy. By coupling knowledge with empathetic encouragement and concrete goal-setting,23 you can help patients find their own personal motivation to stick with the program. Over time, as new routines turn into habits (for example, taking medication becomes as routine as brushing teeth), adherence and healthy behaviors become much easier to maintain.
What practical strategies can improve diabetes medication adherence in resource-limited settings?
Improving adherence in resource-limited settings (common in many emerging countries) involves creativity and community support, in addition to the general strategies discussed. Patients in these settings often face unique challenges such as medication cost, limited healthcare access, and low health literacy. Here are some practical strategies tailored for low-resource environments:
- Enhance Access and Affordability: Cost is a major barrier, so whenever possible prescribe affordable generic medications or those available through public health programs.29 If insulin or certain drugs are scarce or expensive, liaise with local health authorities or NGOs for patient assistance programs.29 In some areas, task shifting to community health workers who can deliver medications to villages or do home visits is an effective strategy to maintain continuity.30
- Utilize Mobile Technology: Mobile phone penetration is high even in many low-income regions, so leverage that. Simple SMS reminders or interactive voice calls in the local language can prompt patients to take their medication and come for refills.11 Mobile health (mHealth) interventions are relatively low-cost and have demonstrated potential to improve medication adherence in chronic diseases.11,12 For example, a weekly text like “Take your diabetes pills every morning – your health is your wealth” can be a helpful nudge. Some programs also use automated calls or chatbot systems to educate patients about their disease and remind them of appointments.
More information about the ‘my a:care’ mobile application: https://acarepro.abbott.com/tools/help-your-patients-take-control-of-their-health-recommend-the-my-acare-app-to-your-patients-now/
- Community and Family Support: In emerging countries, family and community networks are powerful. Encourage patients to involve a family member in their treatment plan, a spouse or child reminding them to take medicine can double as emotional support.31 Community-based support groups or diabetes clubs (even informal gatherings) allow patients to share experiences and tips, which can improve motivation and accountability. If literacy is an issue, pictorial calendars or pill charts can be given to patients and their family caregivers to illustrate when and how to take medications. Training community health volunteers to follow up with patients (for example, checking in on medication supply and understanding) creates a safety net for those who might otherwise “fall through the cracks” of the healthcare system.
- Education tailored to Low Literacy: It’s vital to provide education in a way that patients of all literacy levels can grasp. Use simple language and visual aids – demonstration of how to measure a dose, using pill bottle illustrations for timing (sunrise for morning, moon for night), etc. Culturally appropriate analogies can help convey the importance of adherence (e.g., comparing taking medication to refueling a vehicle regularly to keep it running).32 Repeating key messages at each visit helps reinforce learning. If language barriers exist, involve translators or community elders who can help explain in the patient’s native language.32 Patients are more likely to adhere if they truly understand the purpose of the medication and how it benefits them.
- Address Social Determinants: Be mindful of issues like food insecurity and lack of transport, which can indirectly affect adherence. For instance, a patient who cannot afford proper food may skip medication to avoid hypoglycemia. Connect patients with social support services if available (such as nutritional support or free transport services for clinic visits). Some healthcare centers in low-resource settings establish “adherence clubs” where patients can pick up medications in a group setting in the community, saving clinic trips. These clubs often incorporate brief education and peer support, tackling multiple adherence barriers at once.33
This article was written with the assistance of generative AI technology and reviewed for accuracy.
A: Look for red flags in their behavior and health metrics. Common signs of non-adherence include missed prescription refills or frequent “lost” medications, missed appointments, and persistently poor glycemic control despite an appropriate regimen. Patients may also give subtle cues, for example, hesitating when you ask how they take their medications, or making comments that suggest doubts about the treatment. Directly asking in a non-confrontational way can help uncover issues (“How often do you end up skipping a dose?”). Often, patients who are non-adherent will have one or more identifiable factors like forgetfulness, side-effect complaints, or low understanding of their condition.
More information about a:care Insight: https://acarepro.abbott.com/tools/acare-insight/
More information: A:care masterclass by Dr Sheri Pruitt
https://acarepro.abbott.com/masterclasses/how-healthcare-providers-can-address-non-adherence/
A: This is a common challenge in practice. First, explore cheaper alternatives: prescribe generic versions or alternative medications with similar efficacy that are covered by local health programs or insurance. Many countries have government or NGO-sponsored programs providing essential diabetes drugs at low cost. Connect the patient with those if available. You can also consider simplifying the regimen to reduce cost (for example, using a single combination pill instead of multiple separate pills, if it’s cheaper). Another strategy is to enroll the patient in any patient assistance programs through pharmaceutical companies or charities that provide free or discounted medications. Do not let cost remain a silent barrier. Openly discuss it and involve social workers or pharmacists to help find a solution. By acknowledging the issue and taking action, you show the patient that you are their ally, which itself can improve engagement and adherence.
A: Lifestyle changes are critical in type 2 diabetes management but they usually complement, not replace medications. For patients with early or mild type 2 diabetes, significant improvements in diet, weight loss, and physical activity can sometimes achieve glycemic control to the point of delaying medication need.35 However, for most patients, medications are needed to maintain target blood sugar levels and stopping them completely could lead to loss of control. The best outcomes are seen when patients combine both approaches: taking medication as prescribed and adhering to healthy behaviors such as diet and exercise recommendations.36 Emphasize that medications address the underlying issues (like insulin resistance or insulin deficiency) at a physiological level, while lifestyle changes greatly assist in improving the body’s response and preventing complications. It’s not an either/or situation. It’s both together for optimal health. That said, if a patient is motivated, encourage robust lifestyle changes, as they may allow for lower doses or fewer medications over time under careful monitoring.36
A: Initiating insulin therapy in patients with type 2 diabetes can be challenging, especially when patients are hesitant or outright refuse. Understanding the root causes of resistance is essential for healthcare professionals (HCPs) to guide patients toward effective treatment.
Patients may perceive insulin as a sign of personal failure or disease progression, fear hypoglycaemia or weight gain, or worry about stigma and job security. Others may find the regimen inconvenient or fail to see its benefits, particularly if they’ve not experienced immediate improvements. Poor communication and lack of shared decision-making can further erode trust and adherence.
To address these concerns, HCPs should initiate insulin conversations early in the disease course, framing insulin as a natural and expected step in diabetes management. Active listening, empathy, and open-ended questions help uncover patient fears. Education should be tailored, simple, and ongoing—covering injection techniques, self-monitoring, hypoglycaemia management, and realistic expectations.
Shared decision-making is key. Collaboratively developing a treatment plan that aligns with the patient’s lifestyle and goals fosters ownership and adherence. Frequent follow-up, especially in the early weeks, reinforces progress and provides timely support.
Ultimately, a multidisciplinary approach—engaging educators, pharmacists, and family members—can ease the transition and improve outcomes. By addressing emotional, practical, and informational barriers, HCPs can help patients start and sustain insulin therapy with confidence.37,38
A: It’s important to create a blame-free atmosphere so patients feel safe admitting difficulties. Normalize the behavior when you ask about it. For example, instead of directly saying “Are you taking your medications?”, you could ask, “Many patients have trouble taking their medications every day. How often do you think you miss a dose?”.
More information: A:care masterclass by Dr Sheri Pruitt https://acarepro.abbott.com/masterclasses/how-healthcare-providers-can-address-non-adherence/
This kind of phrasing makes it clear that it’s a common issue and you won’t judge them for honest answers. Listen actively to their response and thank them for sharing. If they admit non-adherence, avoid scolding. Respond with understanding and problem-solving: “Thank you for telling me. Let’s figure out together why it’s been hard and what might help.” If you suspect non-adherence but the patient doesn’t admit it, you can gently probe by asking about their routine: “Walk me through how you take your medications in a typical day.” Also, use objective clues (like pharmacy refill records or A1c trends) to start a conversation: “I notice your A1c is still high; this could be due to many factors, including sometimes missing doses. What do you think might be going on?” The goal is to keep your tone supportive and empathetic, focusing on solutions. When patients feel you’re on their side, they are more likely to open up about challenges, allowing you to provide the help they need.
More information about motivational interviewing: Unlocking adherence: The power of motivational interviewing in medication management













