Health belief model examples for diabetes
- According to the Health Belief Model (HBM), messages that effectively address perceived barriers, benefits self-efficacy, and threats will result in the best behavior change1.
- Although the model appears to be the perfect explanatory framework for communication research, its application in the field has been limited by theoretical constraints1.
What is the health belief model?
The Health Belief Model (HBM) was one of the first models developed in the 1950s, by a group of social psychologists to understand why people engage in or do not engage in disease screening and disease prevention measures2.
There are six constructs of HBM1.
A. Constructs of health belief model1
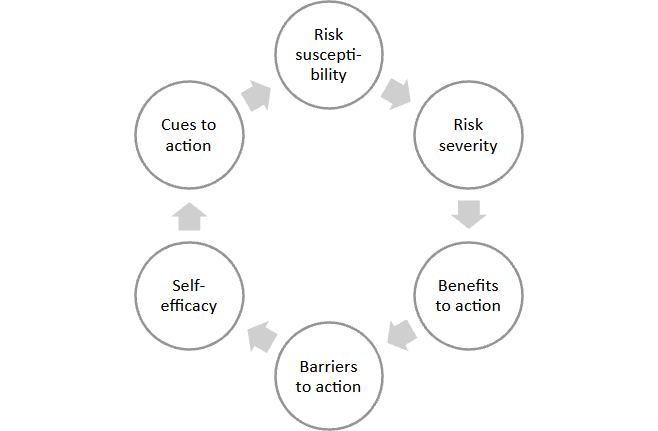
Each of the factors are typically thought to work together additively to affect the likelihood of practicing the behavior. Therefore, it is expected that high susceptibility, high severity, high benefits, and low barrier will result in a high probability of taking the advised action2.
B. What is the health belief model in diabetes
The primary focus of the health belief model is to understand health-related behavior. Generation Y, Z, and Alpha who looks wholesome and active find it difficult to believe they could develop a chronic disease like diabetes; however, to add into their belief and to understand the factor causing an impact on health-related behavior, continuous health education about awareness of disease its incidence and prevalence is utmost important.
The HBM states that people are more likely to take health-related action if they believe and understand susceptibility to an event, its severity, its course of action towards that event, and possible positive benefits and related barriers1.
Diabetes is a chronic metabolic disease3 with silent features. Since there is increased prevalence and less awareness of the disease; HBM could be considered as an effective, efficacious, and comprehensive framework.
Applying health belief model on type 2 diabetic patients
Examining real-world applications of the HBM to diabetes and highlighting how people’s opinions and assumptions influence their behavior regarding self-care might assist to reduce the disease complications3 worldwide.
The construct of Health belief model could be used individually and/or tandemly as an example in diabetes such as:
Example 1: Risk susceptibility, Severity, and Cues to action
Example 2: Benefits and barriers to action
Example 3: Self-efficacy
1. Risk susceptibility, severity, and cues to action
Despite less predictive action of perceived severity towards changing the behavior, studies propose that perceived susceptibility of a disease and its severity could be integratively used along with cues to action for one’s understanding towards threat perception of a disease. Cues to action can be internal or external4, depending on individual effort, event, or some external assistance that triggers change behavior.
To know more about some of the cues to action please read:
“Behavioural approaches to changing adherence” ,
“Patient Support Programs: personalized digital adherence support” and
“Mobile apps for enhancing adherence to chronic diseases”
Note: People are more prone to consider changes as they are exposed to more cues to action.
The majority of people with prediabetes are unaware of their condition, identification and increased awareness of prediabetes are essential first steps in motivating those who have it to adopt healthy lifestyle habits or sign up for programs that promote these changes in order to prevent type 2 diabetes5.
Some of the key points to remember is that merely choosing an approach is not enough until the target understands about the beliefs that how serious the condition is and the related consequences of the condition (perceived severity), the extent to which the individual feels at risk of being exposed/suffering from the condition (perceived susceptibility) and their related action (cues to action).
In the era of today’s world exercise (especially cardio exercise) and physical activity plays an important role in managing diabetes parallelly with diet and medication6. Some studies and clinical trials have shown that in-depth lifestyle modification and physical activity has demonstrated a 58% reduction in diabetes incidence along with prediabetes7.
Despite knowing about the importance of a healthy lifestyle and the role of physical activity to live a longer life people don’t aim to choose it. A sedentary lifestyle is prevalent globally, according to statistics from throughout the world, more than 60% of adults do not engage in the recommended level of physical exercise8, which results in other comorbidities including cardiovascular disease in diabetic patients6 and other chronic diseases.
Coordination of efforts among various stakeholders (Individuals, health professionals, healthcare systems, health payers, community organizations, and public health agencies) is necessary for population-based diabetes screening and preventive methods to be effective in both clinical and community settings as they are collectively responsible for assessing diabetes risk, ordering screening tests, managing screening test results, and engaging in preventive treatments9.
2. Benefits and barriers to action
Perceived barriers and perceived benefits are considered to be the strongest predictors of behavior as reported in the previous studies1,10.To design a community approach for a population or a specific group of community based on HBM; it is important to have a thorough understanding of the basic construct so that perceived benefit takes precedence over other considerations. Health care professional should choose their target population.
Targeting a population (young and energetic) who are less susceptible and not ready to change their behavior would not make much difference rather one should focus on the group (person who have a diabetic patient in the family/peers) who are more susceptible to disease, understand the severity, comorbidities related to the disease and are aiming to change their lifestyle would give a more positive outcome.
There are multiple barriers to diabetes along with non-adherence to the medicine; however, collectively it would be possible to bring down the risk and severity of the disease. To know more please read: “The role of beliefs in non-adherence” and “Medication adherence in patients with type 2 diabetes”.
Despite having an abundance of barriers, there are multiple side effects and comorbidities related to diabetes; however, the training-based HBM model led to an improvement in the scores of perceived susceptibility, perceived severity, perceived benefits, perceived barriers, perceived self-efficacy, cues to action, and physical activity levels8, and building up the confidence to overcome the barriers is essential for everyone.
3. Self-efficacy
People are less likely to act if they think they won’t succeed or that they won’t have any impact. Any program should continually strive to foster self-efficacy by organizing a free campaign for the target audience, continuous awareness about the disease, and positive reinforcement to overcome the disease burden; this joint effort could help build confidence as lack of confidence can be a difficult obstacle to overcome.
Giving compliments and rewarding participation and compliance are two examples of this. To help participants develop their confidence, they could be encouraged to use resources like daily records.
The hardest parts of a diabetes regimen are managing weight and losing it. There are behavior change techniques that have been shown to increase weight loss adherence. Interventions to instruct these techniques have had some degree of success.
- Doctors advise their patients to make specific, attainable goals. In terms of weight management, this implies aiming for losing 2 pounds every week rather than 10 pounds reduction.
- Patients are urged to concentrate on altering their actions rather than their statistics. Instead, then concentrating on how many pounds they have shed, this may entail moving to a low-fat diet.
- They are advised to concentrate on one behavior at a time and begin with tiny, doable steps.
- Patients are educated about the importance of social support and helped to take steps to identify a confidante and ask for help.
Insulin-dependent diabetes
Diabetes is a global health crisis11, and related health and economic burdens have been rising in the past decades.
As per the data availability, the model developed for the prevalence of type 1 diabetes in 2021 reported 8.4 million individuals globally (18% younger than 20 years, 64% were 20-59 years and 19% were ≥60 years). A total of 0.5 million instances of new cases were reported in 2021 (median age of onset: 29 years); out of which ~35 000 undiagnosed people passed away within a year as soon as symptoms began.
It was predicted that by 2040 there would be an increase in cases to 13.5-17.4 million which is more than 50-100% than in the year 2021 in low-income and lower-middle-income countries12.
Health belief model and adolescents’ insulin-dependent diabetes
Adolescents and children are mostly affected by Type 1 diabetes. As per the report, the growing burden of type 1 diabetes is vast12 and the risk of developing the life-threatening condition ketoacidosis13 in adolescents if they have a delayed diagnosis multitiered public health intervention is a need of the hour.
There could be multiple factors of this increasing burden including lifestyle, less awareness about the disease and its symptoms, physical activity, etc; however, healthcare practitioners can assist children and adolescents in developing realistic risk assessments and to overcome those by using the Health Belief Model as a theoretical foundation.
Conclusion
The burden of diabetes is widespread, knowledge of diabetes risk is low, and many persons with prediabetes go undiagnosed as a result of current screening programs. Despite the existence of community-based programs and policies encouraging the development of Diabetes Prevention Programs (DPP) in clinical and community settings.
There is a dearth of infrastructure to support data interchange and referrals between patients, clinical settings, and community-based DPP initiatives. The health belief model has been shown in numerous studies to be effective in helping people comprehend various diseases, the value of physical exercise, and the need of leading a healthy lifestyle for a longer lifespan. However, it may also be a good model for helping people better grasp diabetes and its seriousness.
“Our behaviors reflect what we believe. If we want to change our behavior, we have to change our beliefs.”
― Patty Houser













