The role of beliefs in non-adherence
- Beliefs have a strong influence over a patient’s motivation to adhere to treatment
- These include patient beliefs about their illness, their treatment and their own capacity for adhering (self-efficacy)
- It is vital that clinicians assess patients individually to understand their beliefs and motivations, supporting them in adhering to their medication regimens
Beliefs have an important influence over non-adherence
There are a number of important beliefs that can influence patient non-adherence. These include beliefs about their illness, their treatment, and their own capacity, or self-efficacy, to adhere (the belief that they can successfully perform a specific behavior to achieve a desired outcome).1 In the COM-B framework, beliefs primarily influence adherence via motivation.
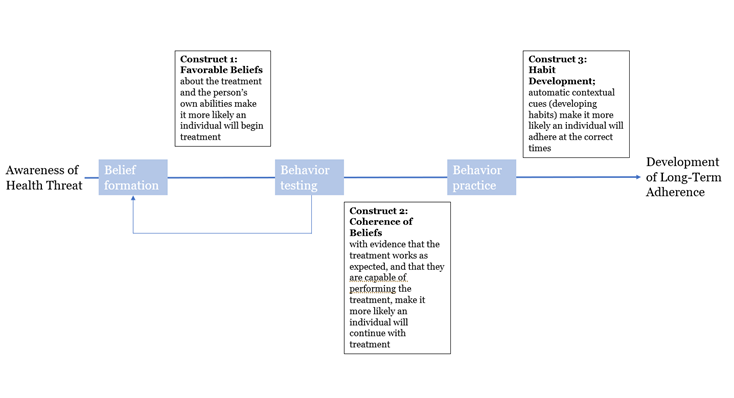
In the long-term, medication adherence is theorized to occur when individuals successfully initiate behavior due to:2
- Forming treatment-favorable beliefs (treatment efficacy and self-efficacy beliefs)
- Receiving experiential feedback/evidence that their beliefs are correct
- Repeating/practicing their medication-taking routine long enough to develop automatic contextual cues that maintain the behavior
Belief-based models
Belief-based models include the Health Belief Model (HBM) and the Theory of Planned Behavior (TPB).
The HBM was designed in the 1950s and has 5 core constructs.3 Perceived severity (beliefs about how serious the condition is and its consequences), perceived susceptibility (the extent to which the individual feels at risk of being exposed/suffering from the condition) and cues to action (internal, e.g. bodily state or symptom, or external, e.g. reminder about doctor’s appointment) all contribute to the individual’s perception of threat. This, in combination with the perceived benefits (effectiveness and availability of taking a particular course of action) and perceived barriers (negative aspects related to following the course of action), contribute to the likelihood of the action being followed.3
The TPB has been widely tested and successfully applied to the understanding of a variety of health behaviors. It has been shown to be predictive of adherence, suggesting that the immediate precursors of a behavior are intentions (i.e. motivation) to engage, which are influenced by a number of factors, including attitude to the behaviour, subjective norms (i.e. what others think) and perceived behavioral control (similar to self-efficacy – see below).4
Beliefs about illness
The common sense self-regulation model (CS-SRM) has been used in many illness contexts to understand the ways in which patients make sense of and cope with their disease. The model describes how individuals develop their own understanding of their illness, or threat to their health, and how this determines their responses, including adherence. Each patient will have their own beliefs about the following factors:2
- Illness identity – the label which the patient uses for their illness and the symptoms which they associate with it
- Causes – the patient’s beliefs about the cause(s) of their illness
- Timeline – the patient’s beliefs about the timeline of their illness, i.e. acute, chronic or cyclical
- Consequences – the patient’s beliefs about the social, cost and health consequences of their illness
- Control – beliefs about how much control the patient thinks they, their doctor and the treatment have
Beliefs about treatment
Taking account of the patient’s beliefs about their prescribed medication is fundamental to understanding and supporting adherence.5
Patient beliefs about their treatment can be grouped into two core themes:6
- The necessity of the prescribed medication for maintaining health at the present time, and into the future
- Concerns about the potential adverse effects of treatment, for example dependence on the medication or long-term adverse events
Evidence has shown that patients who believe in the necessity of their prescribed medication and who have fewer concerns about it are more likely to be adherent.7
Adherence behaviors are influenced by balancing the necessity of the medication for maintaining or improving health against concerns about the potential adverse effects of taking it.5,6
Intentional non-adherence is often based on patients’ correct or incorrect beliefs about beneficial effects, negative side effects or the addiction potential of the medication.8
Beliefs about self-efficacy
Self-efficacy can be defined as someone’s belief or level of confidence that they can successfully perform a specific behavior to achieve a desired outcome.1 Self-efficacy is described as ‘malleable’, i.e. a patient’s levels of self-efficacy can be altered via persuasion or encouragement. It is, therefore, an important pathway to improving adherence to medications.1
Self-efficacy is thought to be one of the most important general predictors of behavior change, and consequently disease self-management (including adherence). 1 A review of published studies in hypertension found that higher self-efficacy was related to better medication adherence.9
Understanding individual beliefs and personalizing patient support
Clinicians should assess individual patients in order to understand their motivations and inherent beliefs. It is useful to discuss these beliefs with the patient if they appear likely to undermine adherence, and educate and encourage belief modification.9 There are a variety of tools available for assessing patient beliefs, including the Brief Illness Perception Questionnaire10 and the Beliefs about Medicines Questionnaire.5 Motivational interviewing may also be a useful tool in helping patients to discuss beliefs and change their behaviors; including asking open-ended questions and focusing on the patient’s personal situations, preferences and values.












