Tackling medication adherence barriers: Improve adherence, reduce societal cost
- Poor medication adherence contributes to worse clinical outcomes and increased healthcare costs across chronic condition1
- Investing in medication adherence reduces the economic burden by lowering healthcare service use and improving quality of life1,2
- Strategies to improve adherence include direct approaches like smart packaging, wearable sensors etc, and indirect solutions such as telemedicine, etc—all aiming to simplify therapy, monitor intake, and enhance access3
Critical role of medication adherence in patient outcomes
As the well-known saying goes, “Drugs do not work in patients who do not take them,” 4 emphasizing an undeniable truth in healthcare. This highlights the critical role of medication adherence in optimizing health outcomes. Adherence is especially important in long-term therapies for chronic conditions such as cardiovascular (CV), pulmonary, and psychiatric etc. According to WHO, adherence to long-term CV and non-CV treatments is low—often less than 50% in low-and middle-income countries.5
The impact of nonadherence is significant, leading to poor therapeutic outcomes, disease progression, and substantial avoidable health care costs.1 For instance, patients with poor medication adherence (<50%) had higher risk of mortality from ischemic heart disease (HR 1.64; 95% CI: 1.16–2.31), cerebral hemorrhage (HR 2.19; 95% CI: 1.28–3.77), and cerebral infarction (HR 1.92; 95% CI: 1.25–2.96) compared to those with good adherence.6 Similarly, medication adherence directly impacts the real-world effectiveness of lipid-lowering drugs, with approximately 22% higher CV events in nonadherent group vs those with good-adherence.7
Figure 1 illustrates the cyclical relationship between medication non-adherence and its downstream economic consequences. Medication non-adherence leads to poor clinical outcomes due to inadequate disease control. This deterioration in health results in enhanced healthcare service utilization, such as increased hospitalizations, emergency visits, and doctor appointments. Consequently, overall healthcare costs rise, and these costs are passed on to patients—often worsening adherence and perpetuating the cycle.1
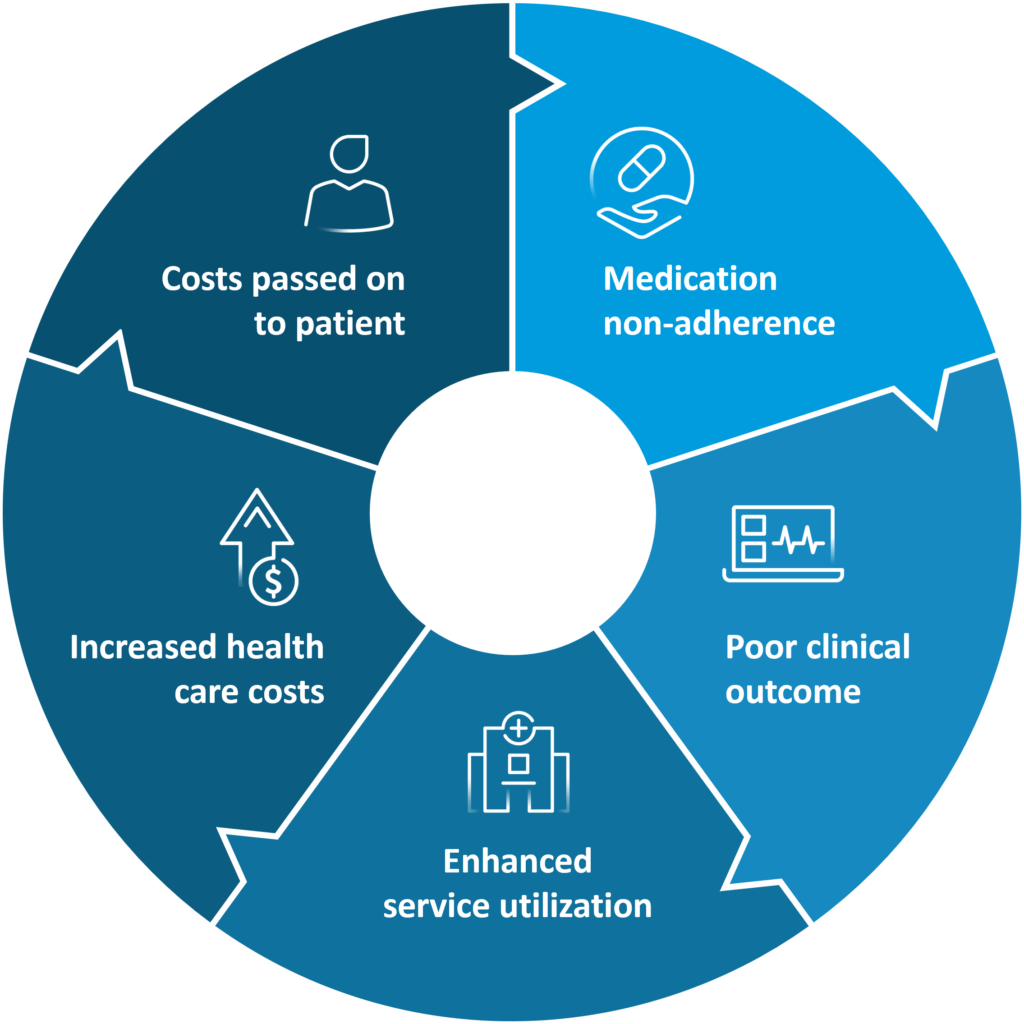
Figure 1: Mechanism that may contribute to medication nonadherence problem within the US healthcare system (Figure is for illustration purposes only and adapted from Iuga AO and McGuire MJ. 20141)
For more details on different barriers of medication nonadherence please read our article: Overcoming barriers to medication adherence: a comprehensive guide
Economic impact of non-adherence
- Medication non-adherence carries a substantial economic burden, encompassing both direct and indirect costs: direct: Immediate impact on medicine acquisition costs; indirect: Less immediate impact, leading to overall health care resource utilization (HCRU) associated with worsening health conditions.8,9
- The financial toll of medication non-adherence is enormous across different regions:
- Non-adherence is estimated to cost $105 billion annually in the US and approximately €125 billion annually in Europe in avoidable direct cost like hospitalizations, emergency care, and outpatient visits.10
- In Australia, total national cost of medication non-adherence across three prevalent disease conditions, hypertension, dyslipidemia, and depression is $10.4 billion annually equating to $517 per adult.11
Economic impact of medication non-adherence on HCRU and work loss (short-term disability, and absenteeism days)
Majority of costs attributed to medication nonadherence result from avoidable hospitalization. It is estimated to cause 10% of all hospitalizations and contribute to $100–300 billion in avoidable healthcare costs annually due to wasted medication and unnecessary diagnostic procedures.12 This also leads to increased HCRU and, as nonadherent patients have higher odds of hospital admissions and accident and emergency visits.13 Similar results of significantly higher hospitalization rates with low medication adherence were observed in a large observational study in the US, involving 135,008 patients with diabetes, hypertension, hyperlipidemia, or congestive heart failure (CHF). Also, higher medication adherence was also linked to significantly fewer annual inpatient hospital days, ranging from 1.18 fewer days per patient for hyperlipidemia to nearly 5.72 fewer days for CHF.14
In addition to medical costs, impact of non-adherence also includes lost productivity due to illness — particularly resulting from absence and disability leaves — imposing cost on patients, their employers and society at large.
For example, employees with diabetes lose 5.4 to 18.1 workdays annually due to absenteeism, compared to 3.4 to 8.7 days for those without diabetes, and up to 78.5 days for those with both diabetes and depression. On average, diabetes adds 2–10 extra absentee days per year, indicating a significant economic burden. Productivity loss is also higher, with 26.3 days lost annually for those with neuropathic symptoms, versus 11.9 days for those without symptoms and 12.0 days for those with no diabetes.15 The large database study that contained data on productivity loss and medical cost of employees of large U.S. employers estimated that employees with type 2 diabetes (T2D) had 4.2 excess days lost than those without T2D. Productivity costs were 13.3% ($680) higher and medical costs were double for employees with T2DM. This contributes to nearly $7,000 higher annual per capita costs.16
Can investing in adherence lead to cost savings?
The high prevalence and consequences of medication non-adherence has led to an era of strategies which can bend down the healthcare cost curve. Evidence from multiple studies have consistently found that improved medication adherence — is not only associated with positive impact on health status of the patients but also confers economic benefit.1,5,17 These mechanisms include direct savings from decreased use of complex and expensive health services needed during disease exacerbation, crisis, or relapse. Indirect savings may come from improved or maintained QoL and the preservation of patients’ social and vocational roles.18
The study was conducted examining the relationship between medication adherence and the use and cost of health services in patients who had one or more of the following four chronic vascular conditions: CHF, hypertension, diabetes, and dyslipidemia. In all four conditions, annual medical spending was significantly lower for adherent patients. In older adults, annual per-person healthcare savings from medication adherence were $7,893 for congestive heart failure, $5,824 for hypertension, $5,170 for diabetes, and $1,847 for dyslipidemia. The corresponding benefit-cost ratios were 8.6:1 for heart failure, 13.5:1 for hypertension, 8.6:1 for diabetes, and 3.8:1 for dyslipidemia.14
Similar findings were observed, supporting the implementation of adherence-enhancing strategies, such as digital interventions, to strengthen secondary prevention efforts in CV disease. Improving adherence can prevent 34–63 CV events per 1000 patients, increase life years and quality-adjusted life years (QALYs), and lead to substantial cost savings from both healthcare and societal perspectives, particularly in middle-income countries such as Mexico, Thailand and China.5
For more details on this HEOR study read our article: JAHA publishes a:care HEOR study: medication adherence yields significant cost savings in cardiovascular disease management
Medicare beneficiaries who adhered to statin medications had twice the odds of achieving better clinical outcomes, fewer healthcare visits, and lower total costs over one year compared to non-adherers, despite higher prescription drug costs. Statin medication adherence was associated with cost savings of $43.49 per patient per month (PMPM) for outpatient costs, $127.57 PMPM for inpatient costs, and $157.32 PMPM for total costs, alongside higher prescription drug costs of $12.69 PMPM, compared to non-adherence over the one-year study period.19 These findings underscore the importance of different strategies in improving adherence, such as digital technologies or behavioral programs, to achieve long-term economic and clinical benefits.
Medication adherence interventions
While no single perfect method exists to improve medication adherence, numerous multifaceted interventions can range from simple educational materials to complex, multicomponent approaches that integrate advanced behavioral and educational techniques.20
- Solutions targeting medication adherence directly3
- Innovative drug designs: Examples include i) fixed-dose combination drugs and polypills; ii) long-acting drugs, reducing pill burden, simplifying drug regimen, and promoting adherence
- Trackable pills: Nano sensor equipped, which allow for direct assessment of medication intake and adherence
- Smart inhalers, injectors, and drug packaging: Assess adherence and share data via mobile applications for (self) monitoring
- Multidose drug packagings, weekly or monthly pill organizers: Preloaded at pharmacy level, these minimize the risk of drug-taking errors
- Smart drug organizers and dispensers: These alert patients of drug intake and notify caregivers in case of non-adherence
- Wearable sensors: Examples include continuous glucose monitoring, smartwatches detecting hearth rhythm and ECG; these encourage (self) monitoring of condition management and thus, help medication adherence
- Automatized appointment reminding systems: Utilize voice calls, email, messaging, etc, for automated appointment reminders
- Mobile/online applications: Various functionalities such as drug identification, knowledge repository, schedule organization, reminders, alerting patient/caregiver/healthcare professional in case of non-adherence, automated drug renewal options, etc
- E-prescribing software solutions: During prescribing process, offer statistics of prescribed, and (less often) dispensed drugs, allowing individual healthcare provider to identify underutilization and overutilization of prescription drugs
- Software analyzing patient’s drug utilization with machine learning: Employ machine learning to analyze a patient’s drug utilization to automatically alert prescribers in case of non-adherence
- Structured drug reviews: Often supported by dedicated software, these are provided by pharmacists or doctors to facilitate deprescribing, enhance adherence, and avoid drug-related problems
- Incentivizing HCP: Incentivize healthcare providers based on achieving certain levels of medication adherence, according to predefined performance indicators
- Solutions targeting medication adherence indirectly3
- Telemedicine/remote consultation options: Facilitate remote consultations, help maintaining continuity of long-term therapies and enable medication adherence
- Electronic prescriptions: Enable the prescription process through electronic means, easing patients’ access to prescription drugs and long-term adherence
- Automatized prescription renewal systems: Enhance prescription renewal processes for improved adherence
- Decision support systems for prescribers: Dedicated software may identify drug-related problems such as drug-drug interactions and potentially inappropriate prescribing, improving overall therapy tolerance
- Online pharmacies and home delivery of prescription drugs: Offer convenient access to medications through online pharmacies and home delivery services
- Big data repositories: Utilize comprehensive data repositories merging prescribing and dispensing data to allow healthcare authorities, payer organizations etc
- Online HCP/medical centers rankings: Provide online rankings to help patients choose HCP and medical centers based on their needs and preferences, and increase their trust
Conclusion
Medication adherence is a multifaceted challenge influenced by both patient-specific behaviors and systemic healthcare factors. Nonadherence to treatment has been a growing concern since the 1970s, with well-documented impact on population health and healthcare costs.18 Medication nonadherence results in significant health consequences, including preventable mortality and global economic burden.17,18 The impact spans from increased healthcare resource utilization to lost productivity, emphasizing the urgent need for targeted strategies.1
Addressing medication non-adherence requires a comprehensive approach, incorporating both direct interventions, such as smart drug technologies and patient monitoring tools, and indirect strategies, including telemedicine support and structured reviews.3 Investing in adherence to treatment not only improves patient health outcomes but also leads to significant cost savings by preventing unnecessary hospitalizations and medical complications. Strengthening collaborative efforts between patients, healthcare providers, and policymakers remains key to mitigating the far-reaching effects of non-adherence on global health systems.18,20
“Improving medication adherence may have a greater influence on the health of our population than the discovery of any new therapy”
— Dr Marie T. Brown; Practicing Internist and Geriatrician













