Connected health devices – the holy grail for improving adherence
- Traditional healthcare models are shifting to digital-first strategies, accelerated by COVID-19, with widespread adoption of connected health technologies worldwide1,2.
- Connected health devices create a digital ecosystem involving patients, caregivers, and practitioners, enabling remote vital sign monitoring, telemedicine diagnoses, and electronic record management3.
- Mobile apps, wearables, smart pill dispensers, and educational platforms reshape patient-centered care, enhancing medication adherence and empowering patients4-6.
- Addressing challenges like data privacy, security threats (replay attacks, External Device Mis-Bonding), regulatory complexities, payers cost constraints and equitable access is crucial for successful integration of connected health devices into healthcare systems7,8.
From tradition to transformation: Navigating the shift
In the recent past, traditional face-to-face healthcare model served as the cornerstone of medical practice, with individuals scheduling appointments with their General Practitioners in response to symptoms or for guidance on health concerns1. This approach changed dramatically with the onset of the global COVID-19 pandemic, which accelerated the adoption of connected health technologies worldwide, prompting a shift to “digital first” strategies in healthcare delivery. Healthcare systems worldwide embraced virtual consultations and connected health systems for patient safety and data sharing2,7.
Consumer behavior reflected this change, with a significant portion of U.S. adults embracing health apps and wearables by 2023, reflecting their value in fostering patient relationships and capturing long-term outcomes8. The projected growth of the medical device market to $94.32 billion by 2026 signals this evolving landscape1.
The rise of connected health: Reshaping patient-centered care
Healthcare professionals have seamlessly transitioned from paper charts to digital resources, utilizing them for remote vital sign monitoring, telemedicine diagnoses, and electronic record management. The essence of healthcare delivery has evolved, with Connected Health at its core. Connected health (CH) extends beyond hardware and software, creating a digital ecosystem involving patients, caregivers, and practitioners3.
Imagine a diabetic patient’s wearable sensor relaying real-time glucose levels to their physician, while an elderly individual’s smart pillbox reminds them to take medication1,9. Connected health with remote monitoring technology heralds a new era of care delivery, enabling providers to monitor patients’ well-being from afar while ensuring their comfort at home. This transformative capability delivers precise, real-time measurements, even during sleep, without burdening patients or healthcare systems. This evolution not only enhances care standards but also allows patients to maintain their daily routines without compromise, marking a significant milestone in healthcare delivery7.
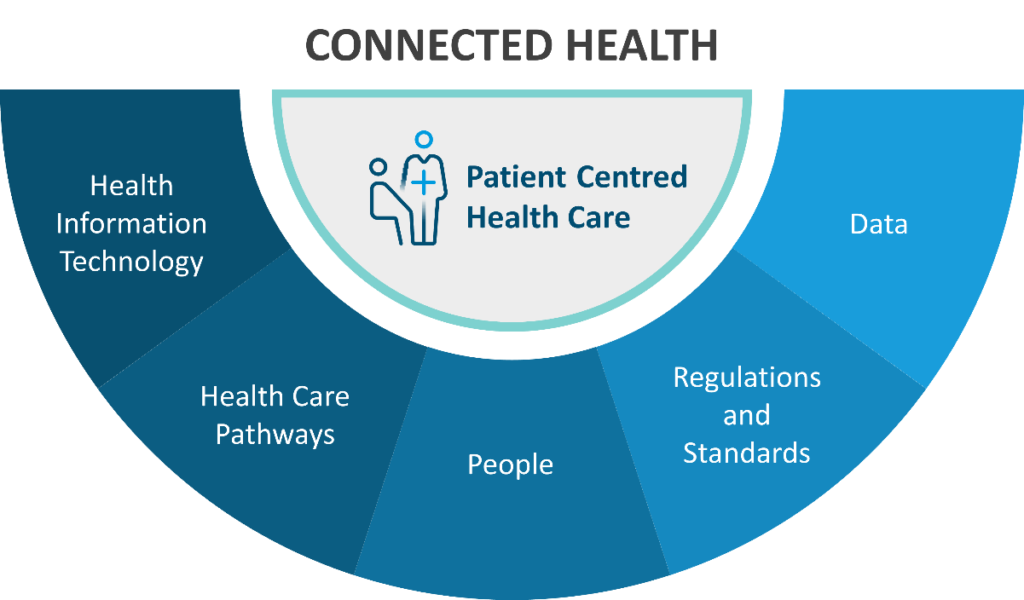
Figure: Connected health components provide patient-centered health care3 (Disclaimer: This image was created for illustrative purposes and is based on data obtained from MacMahon ST. Pathways, technology and the patient-connected health through the lifecycle. Front Digit Health. 2023;5:1057518. doi: 10.3389/fdgth.2023.1057518.)3
Connected Health Devices (CHD) in medication adherence:
CHD leverage technology to empower patients and enhance their adherence to medication regimens. Here are few key types of CHDs:
- Mobile apps: Mobile applications allow patients to set medication reminders, track usage, and communicate with healthcare providers. These apps serve as personalized companions, ensuring patients stay on track with their treatment plans4.
- Wearable devices: Smartwatches, fitness trackers, and other wearables integrate medication reminders and monitoring features. Patients receive real-time alerts and can access information about their medications directly from their wrists2,6.
- Smart pill dispensers: These devices organize medications, dispense doses at the right times, and provide visual or auditory reminders. They are particularly useful for patients with complex medication schedules5.
- Educational platforms: Connected health solutions include educational platforms that provide patients with information about their medications, potential side effects, and proper administration techniques. Educated patients are more likely to adhere to their treatment plans6.
Evidence and effectiveness of connected health devices:
Several studies have explored the impact of CHD, mobile apps on medication adherence. While evidence is still evolving, some findings are noteworthy:
- A meta-analysis indicated that patients using mobile apps for medication support were more likely to self-report adherence compared to those in comparator groups5.
- Patient perceptions of mobile apps have been positive, especially given their automated administration and ease of use10.
Few examples of connected health
- Empowering diabetes management through real-time monitoring
Regular blood glucose monitoring is vital for diabetes care. The Glucose Monitoring System simplifies this with arm placement and a 14-day wear time. Users can scan the sensor to check current levels, trends, and an 8-hour history, stored automatically for easy access11.
A real-world study analyzed data from 1,909 individuals with type 1 diabetes mellitus (T1DM) and 1,813 with type 2 diabetes mellitus (T2DM), including 1,499 on basal-bolus insulin, 189 on basal insulin, and 125 not using insulin. The 24-week real-life use of FLASH among those with suboptimal glycemic control in both T1DM and T2DM showed improvements in glycemic parameters regardless of their pre-use regulation or treatment. Notably, among individuals with T2DM not using insulin and with suboptimal control (TIR < 70%, n = 21; or TAR > 25%, n = 31, with overlap), significant enhancements in estimated Hemoglobin A1c (eHbA1c), time in range (TIR), and time above range (TAR) were observed. These findings contribute to the literature on FLASH utilization, emphasizing its benefits across different treatment modalities and glycemic profiles. Overall, FLASH use for 24 weeks in individuals with T1DM and T2DM showed improved glycemic parameters in most analyses11. - Monitoring blood pressure with telemonitoring
Telemonitoring is pivotal in refining antihypertensive treatment, especially in self-management strategies. Primary-care physicians increasingly rely on self-monitored readings to guide treatment decisions, highlighting its relevance in clinical practice. In the TASMINH4 trial, general practitioners recommending self-monitored blood pressure for medication titration for individuals with inadequately controlled hypertension achieved lower systolic blood pressure compared to titration guided by clinic readings12. Additionally, the study assessed whether adding telemonitoring could enhance self-monitoring’s efficacy. Results showed both approaches reduced blood pressure compared to clinic-based titration. Notably, the telemonitoring group experienced accelerated blood pressure reduction as early as 6 months, suggesting potential benefits in mitigating cardiovascular risks and enhancing long-term blood pressure management. A recent systematic review suggests that self-monitoring enhances adherence to antihypertensive medications13.
Abbott connected health platforms for remote care.
- Cardiac monitoring solutions
Abbott’s Remote Cardiac Monitoring solutions offer a vital connection for those with cardiac conditions14. Utilizing mobile and web applications such as myMerlin™, patients easily engage with their care team. Through tools like Merlin.net PCN and Merlin@home transmitter, remote monitoring ensures efficient device management and timely clinical follow-up without in-person visits. Advances in Merlin.net PCN enhance analysis and patient care. Patients stay seamlessly connected via mobile phones, eliminating manual interaction. Notably, 97% of patients using Abbott’s remote monitoring app comply with the system. - NeuroSphere™ virtual clinic
NeuroSphere™ Digital Care from Abbott is a first-of-its-kind connected care management platform that joins proven neuromodulation therapies with powerful digital health tools15,16. It is the first remote neuromodulation programming technology that includes in-app video chat services. This award-winning platform allows physicians to prescribe and initiate new neurostimulation settings, as well as to optimize therapy directly from Abbott’s Clinician Programmer.
The NeuroSphere™ Virtual Clinic in-app chat streamlines patient follow-up visits. Using the app, physicians can talk with patients about symptoms and outcomes, make real-time therapy adjustments—all without requiring in-person appointments. Physician can access real-time patient-reported outcomes, data, and therapy insights when patients undergo an SCS (spinal cord stimulation) or DRG (dorsal root ganglion) therapy trial period. As patients track and report on pain relief, physicians receive summary reports in real time on their Abbott Clinician Programmer. Physicians receive individual and clinic outcome summary reports—with metrics on pain relief and quality-of-life improvements.
Strategies for Effective Adherence
To maximize the impact of connected health devices, healthcare providers and patients may implement the following strategies:
- Personalization: Tailor adherence solutions to individual patient needs. Customizable reminders, alerts, and educational content ensure that treatment plans seamlessly integrate into daily life17.
- Communication: Encourage open communication between patients and healthcare providers. Connected devices facilitate remote consultations, allowing patients to seek guidance and clarify doubts without physical visits7,18.
- Behavioral Interventions: Behavioral science principles can enhance adherence. Gamification, rewards, and positive reinforcement encourage patients to stay committed to their regimens18.
- Integration with Electronic Health Records (EHR): Connected devices that sync with EHR systems provide a comprehensive view of a patient’s health. This integration enables better coordination among healthcare professionals and ensures continuity of care7,19.
Challenges with connected health devices
- Data privacy:
Privacy and protection of data from CHDs are paramount. Respecting patients’ rights, including access and rectification, is essential. Notably, producers in countries like the United States and Asia may offer differing levels of privacy protection7. - Attacks and device mis-bonding:
CHD providers must tackle data integrity threats for patient safety. Ohno-Machado identifies two key concerns: replay attacks and External Device Mis-Bonding (DMB). In replay attacks, hackers repeat valid data transmissions, like high glucose levels, leading to incorrect insulin doses. DMB risks information leakage and injection, where malicious apps steal data or inject false medical information, endangering patients reliant on health monitoring apps (e.g., blood-sugar concentration, irregular heart rhythm, etc.)7. - Lack of regulatory and legal framework:
Digital technologies revolutionize patient therapy with data from records, wearables, and monitoring devices. Artificial intelligence, machine learning, and big data analytics personalize treatments. Legal complexities pose global challenges. Initiatives like the UK’s National Health Service Long Term Plan target virtual services, yet adoption lags in healthcare and pharmaceutical sectors. Regulatory ambiguity stifles innovation, but agencies like the Medicines and Healthcare Products Regulatory Agency (MHRA) and Food and Drug Administration (FDA) offer guidance7. - Payer, patient, purchaser, and value-based care considerations:
In resource-limited settings, cost constraints underscore the importance of developers finding a balance between simplicity and efficiency in hardware systems7. When it comes to monetizing value, meticulous business model design is critical. Solutions lacking clear economic value for payers will not achieve broad adoption. While goodwill from clinicians and administrators matters, it alone is not enough. If a solution aims to expand market share, it must also provide value to purchasers8. - Equitable access:
Widespread adoption of these technologies requires addressing disparities in access, especially among vulnerable populations7,18. - Integration with healthcare systems:
Senior management must ensure technical readiness, including resource allocation and staff training, for successful integration into clinical practice, where healthcare professionals play a crucial role in educating and advising patients on digital interventions7.
Conclusions:
Advancing medication adherence through connected health devices holds immense potential. By harnessing technology, connect health devices can empower patients, enhance communication, and create a more efficient and patient-centered healthcare ecosystem. As we navigate these innovations, collaboration among healthcare providers, researchers, and patients will be essential to improving adherence and ultimately transforming patient outcomes.
The health gains through virtual connections leading to improved access to medical specialists, better control of chronic health conditions and reduced healthcare costs — could be a silver lining of the pandemic
– Philip Adamson, M.D., Abbott’s chief medical officer













