Community pharmacy interventions for outpatient medication adherence
- Pharmacists are well suited to enhance patients’ adherence to medications because of their accessibility and expertise in the field of medicines1.
- Tailored pharmacy-led interventions can enhance medication adherence by addressing the barriers like socioeconomic, complex regimens, patient concerns, the severity of medical conditions, and health system-related2.
- Pharmacist-led interventions such as medication therapy management, reminders, and motivational interviewing are effective in enhancing medication adherence2-4.
Non-adherence is a common healthcare problem that derails the population’s health outcomes predicted by the treatment efficacy data. It also leads to the failure in translating the highly expensive and time-consuming process of new drug development5 and results in the wastage of prescribed medications. Non-adherence to medication causes an increase in hospitalizations, follow-up visits, usage of higher doses of medication, etc., leading to an overall poorer quality of life for the patients and low efficiency of health systems6.
It is commonly said that “it takes a village to raise a child”. Simply put, any task of significant magnitude calls for a multidimensional approach and teamwork. The World Health Organization (WHO) recommends a multidisciplinary approach to address the multi-pronged issue of medication non-adherence and suggests coordinated action from different stakeholders7. As highlighted in one of our previous articles “Healthcare practitioners: A potential springboard for adherence success”, it takes a team of healthcare practitioners (HCPs), including physicians, nurses, counselors, and pharmacists to make an impact on medication adherence. Community pharmacists exist at the forefront of the patient-HCP interface and are well-positioned to play an important role in enhancing medication adherence notably in an informal setting.
Community pharmacists: The potential “adherence advisors”!
The role of community pharmacists was traditionally limited to dispensing the prescribed medication8. However, now they are being recognized as a crucial member of the multidisciplinary team to tackle non-adherence to medications for complex disorders9. Community pharmacists are ideally suited to provide patient-centered medication adherence interventions10 for the following reasons:
- They are accessible: Pharmacists are easily accessible healthcare professionals8.As per some estimates, visits to pharmacists are more than twice as compared to an HCP11. Pharmacists are in regular contact with patients, especially those who have chronic disorders. This gives them ample chances to build rapport and trust with the patients1.
- Knowledgeable about diseases: Pharmacists have knowledge of disease prevention and management which makes them quite capable of driving several interventions that can enhance medication adherence1.
- Medication experts: Due to their training in pharmaceuticals, they have expertise in different therapeutics. Also, they are well aware of the common side-effects related to a particular therapy and can guide patients in enhancing adherence12,13.
- Understand non-adherence: With their training in pharmacy, they understand the enormity and implications of medication non-adherence11. As they are the actual touch-points for the medication refills, they can be easily trained to monitor medication adherence in their patients and communicate it to the respective physician11,13.
- Familiar with medical devices: The inability to usetherapy-related medical devices like glucometers or inhalers can be a major barrier to treatment adherence. Pharmacists can help patients by demonstrating and managing small technical errors with these devices14.
- Possess a variety of adaptable skills: Due to their training in pharmaceutical and medical science, they possess the basic skill sets for providing health education, managing medications, advising prescribers, and monitoring adherence15.
- Trusted by patients: Pharmacists often count themselves among the most trusted healthcare professionals. Working in informal settings of community pharmacies provides the advantages not offered by structural appointments in a hospital setting. Pharmacists can involve patients to become collaborative participants in making decisions on drug treatment. A public survey revealed that 87% of respondents reported high trust in their pharmacists3,16.
- Can reduce treatment costs: As per the local policies in the United States, pharmacists might substitute prescribed medications with equivalent lower-cost generics with the patient’s consent even without consulting the prescribing physician and therefore can be instrumental in reducing treatment costs17.
The role of community pharmacists was rightfully highlighted during the COVID-19 pandemic when patients, especially those with chronic diseases, relied heavily on community pharmacies for their medication information of over-the-counter and prescribed medications. It also resulted in enhanced trust in community pharmacists with patients reportedly seeking them for more disease-related information18.
Pharmacists-led interventions to enhance medication adherence
In countries like the United Kingdom with a government-supported structured healthcare, pharmacists may assist patients in their medication management by providing medication reviews and assessing medication effectiveness plus safety in a patient-centered manner13. They may also monitor refill adherence and discuss suboptimal medication usage with patients. In addition to these, community pharmacists are also well-suited to provide interventions to enhance medication adherence19. The following section lists a few major pharmacists-led interventions and their impact on medication adherence for chronic diseases in outpatient settings:
- Medication Therapy Management (MTM): The American Pharmacists Association (APhA) defines MTM as a “distinct service or group of services that optimize therapeutic outcomes for individual patients.”. MTM is a patient-centered rather than product-centered approach helping pharmacist assess and evaluate patient’s therapy and other factors20. The intervention comprises the following five elements:
- Medication Therapeutic Review (MTR): Review of medical history, medications, and concerns about medications.
- Intervention and Referral: Identifying concerns and referral to a specialist pharmacist or physician.
- Personalized Medication Record (PMR): An updated list of the prescribed medications, dosage, schedule, and instructions.
- Medication-related Action Plan (MAP): The suggested action plan to mitigate the patient’s concerns for adequate disease management.
- Documentation and Follow-up: Documentation of the services provided, time spent, payments made, and clinical outcomes to be shared with the doctor and payer20.
- Evidently, a pharmacist-led MTM intervention in chronic kidney disease patients resulted in a significant reduction in poor medication adherence (67.8% to 43.1%; p<0.001) and a decrease in usage of non-steroidal anti-inflammatory drugs (19.8% to 8.4%; p<0.001) 21.
- Motivational Interviewing (MI)
It is an evidence-based method of communication that is direct, collaborative, and patient-centered. It elicits behavioral change in patients by activating their internal motivation to adhere to their medication3.The four core processes of motivational interviewing are Engaging, Focusing, Evoking and Planning (Figure 1). Further, the four main skills required for delivering MI are open questioning, affirmations, reflections, and summaries22 as shown in (Figure 1).Pharmacists can be trained to identify and deliver MI interventions to non-adherent patients. Combined results from several studies on patients with cardiovascular diseases receiving community pharmacy-led MI interventions demonstrated significant improvement in medication adherence (p<0.05)3.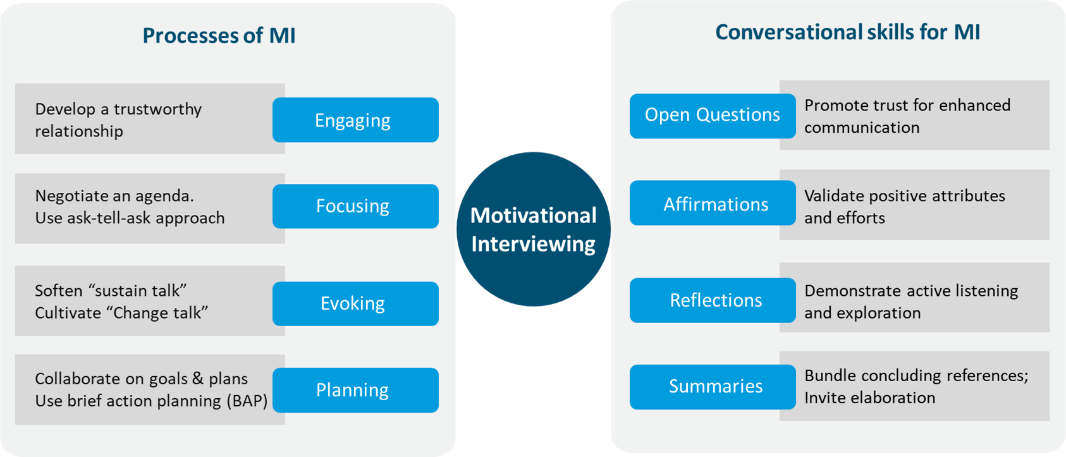
Figure 1: The processes and skills required for delivering motivational interviewing (MI). (The figure is adapted from Cole et al., 202322 and is for illustration purposes only.)
To learn more about techniques for addressing non-adherence through MI, please see How healthcare providers can address non-adherence.
- Patient Education
Educating patients about medication, disease, side effects, and device usage is important to underscore the significance of prescribed treatment and countering non-adherence. It prepares them to manage medication-related adverse effects and use medication devices correctly23. Due to their close ties with the community, pharmacists can communicate with patients using empathy and acknowledging their struggles in using medication. They can deliver patient education with dignity, respect, and personal understanding24.
Pharmacist-led education programs for diabetic patients in an Indonesian cohort improved patients’ knowledge by 19.2% (p = 0.409) and medication adherence, by 46.1% (p = 0.002) 4. - Generic substitutions to reduce medication costs
The cost of medication therapy is a key barrier to medication adherence. The use of generic medication in chronic diseases is reported to enhance adherence to therapy25. To learn more about generics and their role in enhancing medication adherence, please read “Prescription costs are key to non-adherence: Can generics help?”
Being in charge of dispensing the prescribed medication and refills, pharmacists hold the key to reducing treatment costs. They can help patients by substituting generic medication with their consent17. - Other measures
Some other measures like appointment-based models, collaborative practice agreements, and text messages are also helpful in increasing adherence. In the appointment-based model, pre-prepared refills for dispensing allow additional time for patient education and counseling. Collaborative practice agreements between the prescriber and the pharmacists help in easy generic substitutions. Text messages with reminders help in MTM2.
Table 1: Studies demonstrating positive impact of pharmacist-led interventions on medication adherence.
| Therapeutic Area | Intervention | Improvement in Medication Adherence |
|---|---|---|
| Dyslipidemia, diabetes, hypertension | Motivational, educational, reminders | The mean PDC increased by 14% (p<0.0001)26 |
| Cardiovascular disease | MI | Significant improvement in medication adherence (p<0.05)3 |
| Major Depressive Disorder | Educational and medication reminders | Adherence rate improved at 6 months when compared to control: 55% vs 15.2% (p<0.0001)27 |
| Chronic Kidney disease | MTM | Significant reduction in medication non-adherence (67.8% to 43.1%; p<0.001)21 |
| Asthma | Pharmaceutical counseling | Significant improvement in medication adherence (p<0.05)28 |
| Osteoporosis, hypertension, diabetes, depression | Telephone counseling and motivation | Positive impact on adherence29 |
CTT: Controlled-to-total ratio; PDC: Proportion of days covered
How can healthcare systems help community pharmacies in providing care?
Although community pharmacies are well poised to address the challenge of medication adherence, they need to be suitably supported by the healthcare system. This will facilitate the success of pharmacy-led intervention and their widespread application. Some of these measures are:
- Need to recognize pharmacists as bona fide healthcare providers:
Community pharmacists are often the first touchpoint while availing medical care. Even then they are not always endorsed as healthcare practitioners. Therefore, currently, not all medical insurance providers, for example Medicare (United States), cover pharmacist-led interventions. Recognizing them as healthcare providers by policymakers will ensure that their services are optimally utilized across all care settings. This will help them to be directly reimbursed and incentivized for pharmacist-led health services11. - Training and upskilling pharmacists:
Pharmacists need to be abreast with information about different diseases, medications, and treatment-related issues likely to be faced by the patient. Regular education on new drugs, medication devices, costs of generics/branded, pros, and cons of each drug, can help them to influence patient’s ability to adhere to the medications24. - Incentives and payments:
Pharmacists can be incentivized to ensure quality services. One such example is performance-based pharmacy payment models (PBPPM) used in the United States. This uses factors like medication adherence rates, generic drug utilization, frequency of hospitalizations, formulary compliance rate, etc. to appropriately incentivize pharmacies for their work by the payers30.
Interprofessional medication management: Potential for community pharmacists
Pharmacists are beginning to be included as members of the interdisciplinary care provider team in general practice31. However, the role of community pharmacists can not be undermined to tackle the enormous yet preventable global health problem of non-adherence. Their accessibility and expertise in the field of medications combined with informal settings of community pharmacies gives them a unique advantage to involve patients to become collaborative participants in making decisions on drug treatment as demonstrated by the positive impact of community pharmacy-led interventions in enhancing adherence.
Incidentally, it’s easy to write prescriptions, but difficult to come to an understanding with people.
– Franz Kafka (A Country Doctor), author













