The role of patient autonomy in medication adherence
- Autonomy drives adherence: Patient autonomy allows individuals to make informed, voluntary healthcare decisions which align with their personal values.1,6 Thus, patient take ownership of their care leading to better engagement and can promote adherence.1,7
- Factors shaping patient autonomy: Autonomy is influenced by factors like complex information, mental capacity, culture, family support, communication, and health literacy.3,7-8
- Communication builds trust: Empathetic dialogue, supported by tools helps physicians identify behavioral barriers early and tailor communication for personalized care.8,9
- Challenges remain: Shared decision-making boosts outcomes, but short consultation time, medical jargon, cultural gaps and emergencies still limit true autonomy in practice.7
Introduction: Communication as the cornerstone of patient autonomy
Quality care starts with meaningful dialogues, well before any prescription is issued. When patients take part in the decision-making process, they feel empowered to make informed choices.1 This can lead to better adherence to their medications.1
Patient autonomy is not limited to a signature on a consent form or choosing from available treatment options.2,3 It includes liberty to accept or reject care.4 Autonomy also involved access to clear understandable information, respect for personal values and preferences throughout their health journey.4,5,6
This article puts communication at the heart of supporting patient autonomy. It explores how autonomy directly impacts medication adherence. Real-world factors that influence autonomy and common barriers to patient engagement. Finally, the article offers practical strategies for physicians to support active patient participation in treatment decisions.
A:care Insight: Empowering conversations that drive adherence
Rather than waiting to find out why a patient struggles with adherence, a:care Insight helps physicians act early. It allows physicians to proactively identify behavioral, emotional, and social drivers of non-adherence, before treatment begins. Each patient faces different barriers to adherence i.e., difficulty seeing future benefits, feeling disconnected, or reacting to perceived authority. It helps identifying these barriers and allow physicians to develop tailored conversations, build trust, and support patients in making informed treatment choices. For detailed exploration please read our article: a:care insight.
Why autonomy and dialogue are essential for adherence?
Autonomy isn’t simply a good-to-have concept, it is a strong factor that can predict if patients will comply with their medication regimen.4 When individuals are given opportunity to be involved in decisions about their health, they comprehend well with treatment and willingly follow their treatment plans.3,8 Ownership of taking decisions develop accountability and people stay actively engaged in their care.7
Conversely, patients who feel sidelined or coerced are more likely to skip or stop their medications, even if it is very effective or necessary.4 Nevertheless, valuing autonomy does not mean that patients will always take their treatment. Informed and well-supported patients may choose to discontinue treatment.1 This can be due to the following reasons:
- Informed refusal: Patients when acquainted about the medication risks-benefits and alternatives; they can evaluate if risks outweigh benefits. Thus, may then choose not to continue with their treatment.1,4
- Side effects and burden: Patients may logically decide not to receive treatment because of the inconvenience or side effects or financial concerns.2,4
- Medical goals versus personal priorities: Patients often give higher importance to their quality of life, comfort, or personal goals than to medical objectives, which may result in decreased adherence.4
- Autonomy versus beneficence: Physicians may advocate for medical outcomes that do not align with patients’ values. Moreover, recommending treatment without addressing these preferences compromise patients’ true interests.4
Factors that shape patient autonomy
There are several factors which can influence autonomy to make informed decisions about their care (also depicted in Figure 1):
- Understanding and clarity: Patient should have clear and truthful information that is free from medical jargon. Information in plain language about their diagnosis, prognosis, potential interventions, alternatives, and associated risks and benefits to make informed choices.7-9
- Emotional and mental state: Patients that are distressed, sad, or emotionally overloaded may struggle to make decisions. Psychiatric illnesses and cognitive impairments can make understanding complicated information even tougher. In these circumstances, decisions may be made with the help of extra support from family or professional advocates.8,9
- Influence from religion and cultural: Cultural competence means being aware of and sensitive to the differences in the way think, communicate, and make decisions.7-9 In Western healthcare, often significant emphasis is given on individual autonomy, meaning that patients often make their own choice. However, in many non-Western cultures, family plays a central role in major decision especially when related to health. Physicians may decide to refrain from disclosing serious diagnoses out of respect for these collective values. In many cases, religious or spiritual convictions, can impact treatment decisions.9
- Family and social support: Family and social network support can be both a strength or a vulnerability. When patients feel supported by people who understand their values, autonomy grows. Autonomy, however, may not be entirely voluntary if there is undue influence or pressure by family. These situations need to be managed delicately by health professionals from an ethical perspective.8,9
- Relationship and communication style: Patients are more likely to be motivated and adhere to their treatment plans better, when they feel heard by their physicians.8 Open-ended inquiry, mirroring remarks, and culturally sensitive communication strategies such as A:care insight are just a few of the techniques that have been demonstrated to help doctors improve understanding and trust.9 Respectful communication with families and efforts to address language barriers can also help to promote patient autonomy and shared decision-making.8
- Health literacy and resource accessibility: To make decisions on their own, people require a certain degree of health literacy, education and system understanding. Patients with higher health literacy and access to resources tend to be more engaged and autonomous.3,7 But when people lack that knowledge or support, their ability to make truly informed decisions can be limited.3,7
- Special populations (children, elderly, mental health): For kids, autonomy grows over time and must be balanced with parental guidance.9 Elderly patients face unique vulnerabilities involving cognitive or social factors challenges that affect decision-making and safety. People living with serious mental illness may struggle to advocate for themselves unless systems like psychiatric advance directives or peer-support models are placed to protect and empower their choices.9
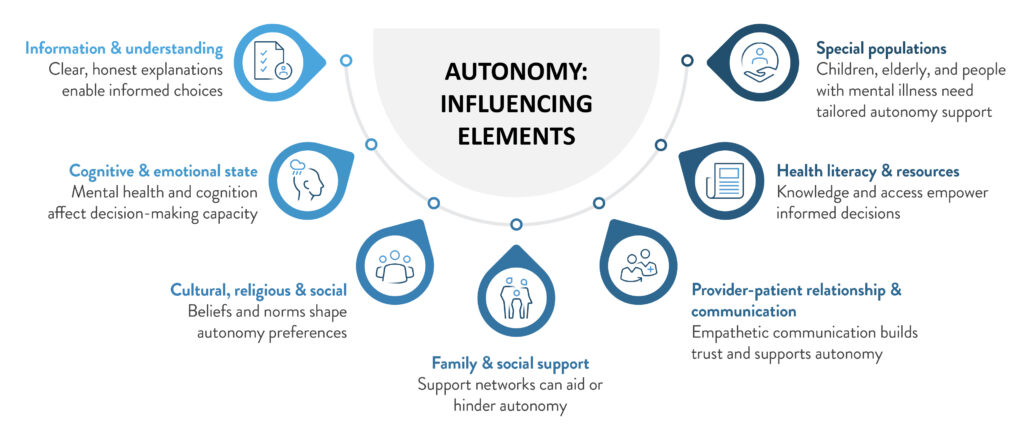
Figure 1: Key factors shaping patient’s autonomy
(The image is only for illustration purposes and the content is from Woodruff J. 2023, Katz JM. 2025, Gumban RJ. 2024 and Moran M. 2025.3,7-9)
Strategies to foster patient autonomy
Practical interventions that are multifaceted are required to help patients feel empowered in making decisions about their care. Key evidence-based strategies summarized in Table 1. They provide methods for establishing a clinical setting that supports autonomy which increases patient satisfaction engagement and treatment compliance.
Table 1: Approaches to enhance patient autonomy
| Strategy category | Key actions to foster autonomy |
| Improving health literacy7,8 | Provide clear, comprehensive information about medical conditions and therapies. In order to foster informed engagement, encourage patients to investigate topics and to ask questions. Utilize accessible digital health tools, apps and online platforms that promote self-monitoring. |
| Empowering patients7-9 | – Build trust and mutual respect through active listening. – Clearly communicate the costs and available treatment options. – Engage patients in collaborative decision-making, respecting their preferences and priorities. |
| Enhancing communication7-9 | – Practice active listening, empathy. – Use clear explanations and confirm understanding. – Employ tools to develop communication strategies. |
| Practicing cultural competence7-9 | – Ask patients preferences for information sharing and decision participation. – Respect cultural, religious, and social values while avoiding assumptions. – Offer interpreter services and continually reflect on implicit biases. |
| Involving family and social support9 | – With patient consent, engage family or trusted supporters as resources for decision-making. – Guard against coercion and ensure patient preferences remain paramount. |
| Addressing power imbalances9 | – Acknowledge and reduce professional hierarchies to encourage open communication. – Prove a safe environment for underrepresented voices to express grievance or disagreement. – Promote relational autonomy by acknowledging social and cultural identity factors. |
| Leveraging decision aids and technology3,8 | – Use brochures, videos, and online tools to clarify options and outcomes. – Provide organizational tools and reminders for self-management, controlled by patients. |
Evidence: When communication and autonomy align, adherence improves
These examples illustrate that encouraging autonomy is a crucial factor in adherence and fruitful clinical outcomes across diverse populations:
- Type 2 diabetes (n=326 Veterans): Patients with substantial autonomy support from a friend or family member reported higher self-efficacy (linear regression coefficient beta, B = 0.81) and less diabetes-related distress (B = -0.32). Monitoring of blood glucose increased (B = 0.29, p < .001). Glycemic control improved even after a year (after adjusting for age, race, insulin use, and patient-supporter relationship; reduced HbA1c, B = -0.25, p = 0.003). However, there was no significant impact on medication adherence (B = 0.003, p = 0.87). Hence, a respectful, autonomy-supportive relationships can have favorable impact in diabetes care.10
- Chronic kidney disease (n=56 providers): Dialysis provider autonomy support was found to be poor in a cross-sectional study, with variations by role of dialysis provider. Only 25% of physicians and nurse practitioners reported actively listening to patient preferences, while 19% of technicians offered the highest level of support. Only 50% of providers tried to understand patients’ views before making changes. Strong correlations were observed between autonomy support score and attitudes toward education and communication (Pearson correlation coefficient, r = 0.40, p = 0.003), counseling confidence (r = 0.64, p < 0.005), and accountability for handling nonadherence (r = 0.69, p < 0.005). Therefore, improving adherence may require specialized assistance that promotes patient autonomy and guarantees reliable patient-centered care.11
- Hypertension (n=75): Patients who sought active or shared decision-making exhibited higher adherence (89.3% and 83.8%, respectively) as compared to passive decision-makers (63.0%). Patients who preferred shared or active decision-making were more likely to comply with medication versus those who preferred to defer decisions to their provider (linear regression coefficient beta i.e. B = 15.87, p = 0.02; and B = 22.58, p = 0.004, respectively). The association between decision-making preferences and adherence persisted even after controlling for patient demographics and provider characterstics.12
- Atrial fibrillation (n=52): In case of atrial fibrillation, patient anxiety dropped from 3.56 to 2.92 (p < 0.001) after a shared decision-making (SDM) consultation. The number of patients willing to begin oral anticoagulants increased from 76.9% to 88.5%, while patients having uncertainty decreased from 15.4% to 1.9% (p = 0.006). Interestingly, gender had an impact on anxiety reduction (p = 0.025), with women benefiting more from consultations. These findings suggest that SDM help patients with atrial fibrillation better understand their treatment options, feel less anxious and make better decisions.13
- Multiple Sclerosis: Studies indicate that patients with multiple sclerosis who feel informed and involved in their medication choices are more likely to remain on treatment. Communication gap between providers and patients are major factor for nonadherence.14
Breaking barriers: Communication as a path to autonomy
Several factors can still hinder communication, even with the best intentions as below:
- Time constraints: Short clinician-patient consultation time reduces opportunities for meaningful conversations. Patients may hesitate to engage fully, making shared decision-making harder and thus unintentionally limiting autonomy in practice.7
- Complex medical information: Medical jargon can be confusing and overwhelming especially during acute or emergency situations. This makes it tough for patient to fully understand their options and take informed decisions.7
- Cultural and language barriers: Communication can be challenging when patients and healthcare providers come from diverse cultural or linguistic backgrounds. At times, families may request non-disclosure of information with patient. This place physicians in difficult ethical situations where they must balance cultural sensitivity with the patient’s right.7
- Emergent and public health crises: During public health emergencies, like COVID-19, individual autonomy may need to be balanced against the safety of the broader community. These situations can temporarily limit personal choice.7
Conclusion
Medication adherence is built on partnership and not just prescription. When physicians listen with intent and tailor conversations using behavioral insight, patients feel respected, understood, and empowered. With that understanding in place, autonomy is not merely an ethical checkbox. It becomes the foundation for treatment plans where patients are willing and motivated to follow. When communication is thoughtful and respectful, it upholds autonomy and makes care feel more personal. This build trust leading to better adherence and improved outcomes.













