Understanding the challenge of adherence in pancreatic exocrine insufficiency
- Pancreatic exocrine insufficiency poses a significant burden on the lives of those affected
- Adherence to medications is challenging due to regimens that require precise dose and timing
- Collaboration between healthcare provider and patient is important to reinforce adherence as a positive behavior
Pancreatic exocrine insufficiency is associated with several conditions
Pancreatic exocrine insufficiency (PEI) is defined by insufficient secretion or function of pancreatic enzymes or sodium bicarbonate for normal digestion.1,2 Its prevalence in the general population is unclear, and estimations are problematic due to the lack of a suitable screening test.1 It is, however, accepted that prevalence of PEI increases with age, and is estimated to be as high as 11.5–20% in apparently healthy older individuals.1
Common causes of PEI include:
- cystic fibrosis3,4
- chronic pancreatitis3,4
- pancreatic cancer3,4
- upper GI and pancreatic surgery4
Half of those who have had chronic pancreatitis for five-to-ten years will develop PEI and 4/5 of those with severe chronic pancreatitis have PEI.3 A systematic review and meta-analysis found that 73% of patients with advanced pancreatic cancer had PEI and that treatment of the PEI was associated with significantly longer survival, compared with no treatment (12.6 vs. 8.7 months, p=0.002),5 underlining the importance of adherence to treatment in achieving the best outcomes for these patients.
PEI medication imposes a substantial burden on patients
Pancreatic enzyme replacement therapy (PERT) is the main pharmacological treatment for PEI, with the primary treatment goal of eliminating maldigestion/malabsorption and maintaining adequate nutrition.6,7 Modern preparations contain pancreatic extract encapsulated in microtablets or microspheres with pH sensitive enteric coating.2,6
The advantages of PERT include helping to manage symptoms of digestive problems (e.g. weight loss, diarrhea) and helping patients to cope better with other treatments (e.g. chemotherapy, surgery). Managing problems with digestion can improve patient quality of life.3,8
In those patients who seem to be failing therapy, the most common reason is non- compliance9,10 (sometimes owing to cost), wrong timing of ingestion9,10, or inadequate dosage.9,10
Defining adherence
Adherence is a key factor in the effectiveness of therapies for both chronic and acute diseases.
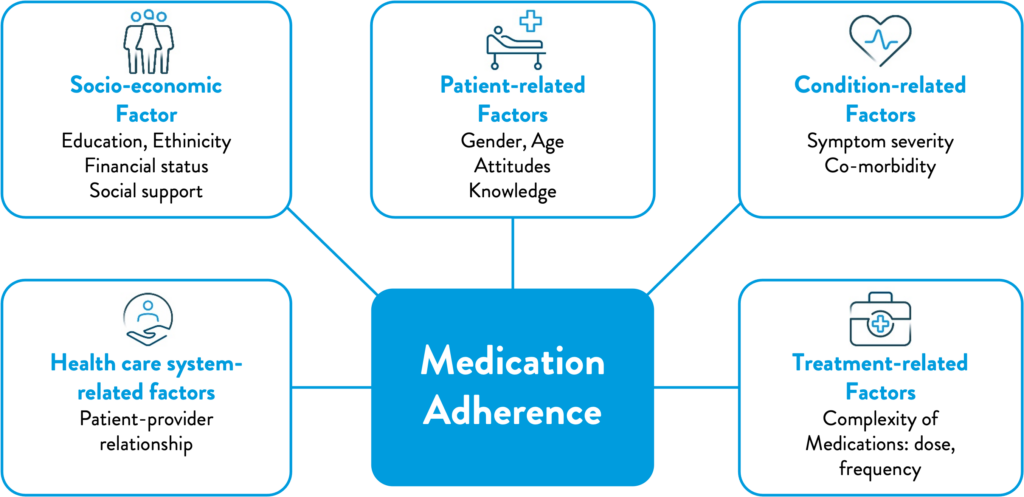
The definition has evolved since an initial description was mooted by the WHO in 2001: ‘the extent to which patients follow medical instructions’. It has since been extended to encompass the range of medical interventions used to treat chronic diseases, and highlight the importance of the relationship between the healthcare provider and the patient, leading to the development of a multidimensional adherence model.11
Figure 1: WHO multidimensional adherence model2
There are multiple stages and types of adherence; it can be differentiated between intentional and unintentional behaviors.12 Intentional non-adherence describes an active decision by a patient not to take their prescribed therapy. Unintentional non-adherence is a passive process, where patients fail to follow prescribing instructions either by forgetting to do so, or due to circumstances that are beyond their control – this form of non-adherence is thought to account for between 20 and 50% of patients.12 There is not always a clear line between the two; it has been suggested that unintentional non-adherence can be influenced by the patient’s beliefs about their medication, presence of chronic disease and other socio- demographic factors, which may also influence intentional non-adherence in the future.12
Non-adherence is therefore not classified as a single behavior. It encompasses multiple stages:13
• Initiation (Fulfillment)
The patient takes the first dose of their prescribed medication.
• Implementation (Compliance)
Defines the extent to which a patient’s actual dosing corresponds to the prescribed dosing regimen
• Persistence
The length of time between initiation and the last dose that immediately precedes discontinuation
Non-adherence in PEI
Management of PEI has been shown to be suboptimal in an analysis of 5,358 patients with chronic pancreatitis, pancreatic cancer, and pancreatectomy. A large proportion of patients was found to be non-adherent to their PERT regimen, and this was found to be associated with higher utilization and healthcare costs.14 European guidelines regard ‘adequate and appropriate PERT’ as essential in the management of chronic pancreatitis.15
Compliance with PERT administration guidelines has also been shown to be low among patients with pancreatic cancer; however, improvement in symptoms significantly correlated with appropriate use of PERT.16
The consequences of non-adherence, and how to mitigate these
The consequences of not only not taking medications, but of taking them inappropriately, can be severe. Medication-related problems can result from taking an inappropriate dose, missing doses or from drug-drug interactions.17
Non-adherence to PERT in the management of PEI has been shown to be associated with higher utilization and healthcare costs.14 The complexity of dosing may be partly mitigated by educating patients on dosing strategies and reducing pill burden.18
An extended clinical care team, including nurses,19 pharmacists20 and dieticians19,21 can provide additional support and education to optimize patients’ adherence to their therapies.
There are a number of behavioral frameworks and tools that can be utilized to improve adherence, including patients support programs (PSPs).
Early models were simple and relied on written interventions to improve adherence in the short term. This later progressed to educating patients, both about their disease and interventions, with follow up from healthcare professionals to improve long-term adherence.22 The generally accepted ‘gold standard’ now involves the measurement of adherence using digital tools, enabling personalized interventions and collaboration between healthcare professional and patient.23
These models and tools will be discussed further in subsequent articles in this series.





