Interprofessional collaboration for medication adherence in diabetes management
- Diabetes, a chronic metabolic disorder1,2, has a high comorbidity burden3 resulting in polypharmacy and increased barriers to medication adherence4.
- A comprehensive medication management program5 and interprofessional collaboration between physicians, pharmacists, and insurance providers is pivotal for addressing this issue6.
Diabetes is a major health problem that is growing at an alarming pace1. Globally, 1 in 11 adults has diabetes (90% have Type 2 diabetes mellitus) and its prevalence is expected to increase from 415 to 642 million by 20402. It was the seventh leading cause of death worldwide resulting in the loss of 1.6 million lives in 20163.
Diabetes is associated with a high medication burden such as cardioprotective medication, as well as other drug classes such as medicines for kidney diseases, neuropathies, depression, and gastric symptoms4. More than 40% of T2DM patients are reported to have 3 or more comorbidities7. Individuals with diabetes faces significant medication burden, with most taking between 4 to 10 medications each day4. The burden of additional chronic conditions significantly complicates diabetes management in patients3.
Polypharmacy: A catch-22 situation in adherence to diabetes treatment
Diabetes treatment is marred with lower rates of adherence. A study reported range of 6.9%-90.6% prevalence of non-adherence. This may also lead to higher morbidity and mortality8. The chronic nature of the disease as well as the presence of comorbidities results in polypharmacy and complex treatment regimen which in turn may lead to higher rates of side-effects leading to a higher likelihood of non-adherence to the treatment4. To understand various barriers to non-adherence to diabetic medications and the relevant interventions, please read our article “Medication adherence in patients with type 2 diabetes: barriers & interventions”.
Medication management programs: A “must have” for diabetes treatment
Due to the high prevalence of medication use and polypharmacy, it is imperative to use comprehensive medication management programs for diabetes treatment. Medication management is “patient-centered care to optimize safe, effective, and appropriate drug therapy” 5. Pharmacist led medication therapy management clinics in US have been shown to improve health outcomes by reducing costs in several chronic health conditions9.
As discussed in one of our previous articles, Community pharmacy interventions for outpatient medication adherence, the intervention comprises the following five elements10 and is usually provided by pharmacists:
- Medication Therapeutic Review (MTR): Review of medical history, medications, and concerns about medications10.
- Intervention and Referral: Identifying concerns and referral to a specialist pharmacist or physician10.
- Personalized Medication Record (PMR): An updated list of the prescribed medications, dosage, schedule, and instructions10.
- Medication-related Action Plan (MAP): The suggested action plan to mitigate the patient’s concerns for adequate disease management10.
- Documentation and Follow-up: Documentation of the services provided, time spent, payments made, and clinical outcomes to be shared with the doctor and payer10.
Polypharmacy, defined as the concurrent use of multiple medications, is associated with negative outcomes such as nonadherence, drug interactions, inappropriate prescriptions, and a higher risk of hospitalization and mortality11. Effective strategies to manage polypharmacy in diabetic patients could improve patient’s quality of life and adherence to therapy11,12.
Interprofessional collaboration: A prerequisite for effective diabetes management
Interprofessional collaboration practice (ICP) is defined as a set-up where “multiple health workers from different professional backgrounds work together with patients, families, carers, and communities to deliver the highest quality of care” 6. Interprofessional care is crucial to achieving quadruple aim of “improving patient health, enhancing patient experience, reducing health care costs, and improving the work life of providers and staff” 6. Collaboration is necessary to coordinate between multidisciplinary teams and for shared decision-making13. It can enhance the delivery of patient-centered care and lead to improved outcomes14.
The core components for the successful implementation of interprofessional collaboration are role clarity, shared decision-making, interprofessional values and ethics, and conflict resolution as well as communication and reflection14 as listed in the figure 1:

Figure 1: The core components for successful implementation of interprofessional collaboration in healthcare.( This figure was created for illustrative purposes and is based on data obtained from McLaney E, Morassaei S, Hughes L, et al.)14.
Clinical studies from both high-income and middle-low-income countries have demonstrated the usefulness of ICP in improving glycemic levels, quality-of-life, and reducing cost of care13. In the following sections, we discuss the role of different stakeholders such as general practitioners, pharmacists, and insurance providers in collaborative medication management for diabetes care.
Role of Primary care clinician (PCCs):
Primary care clinician serve as the first line of care for diabetic patients, developing treatment plans and monitoring patients’ overall health15. Collaboration between physicians and pharmacists on medication management can improve treatment outcomes 16.
As per the Centre for Disease Control (US), physicians can promote medication management in their patients by orienting them to medication management practices by pharmacists and briefing them about the pharmacist’s role in healthcare teams. The action plan recommended for physicians to help their patients are the following16:
- Acknowledge the higher risk of medication-related problems in patients with diabetes.
- Use collaborative drug therapy management (CDTM) in treatment plans for diabetic patients.
- Generate medication awareness by enquiring about all the medicines taken by patients and seeking updates on medication reviews by pharmacists.
- Help patients see the connection between diabetes management and medication management.
- Refer patients to diabetes self-management education and support (DSMES) services.
Contributions of Pharmacists:
Pharmacists are integral members of the healthcare team. They offer expertise in medication management and adherence and help patients get the most benefit out of their medicines. They work directly with GPs to identify, prevent, and resolve problems related to medicines. This partnership is called collaborative drug therapy management (CDTM) 16.
Pharmacist-led medication review and medication management programs (MMP) are well-known strategies to improve medication safety and effectiveness17. Collaborating with GPs, pharmacists can provide medication therapy management (MTM) services tailored to diabetic patients18,19. In addition, they can provide information about the lower-cost options available for medicines and medical supplies16.
Role of Pharmacists to lead CDTM16:
- Conducting comprehensive reviews of medicines and medical records.
- Educating patients for safe and appropriate use of medicines.
- Assessing patients’ responses to therapy to ensure timely interventions.
- Coordinating with primary care and other providers and continuity of patient care.
- Educating patients on how to safely use their medicines and blood glucose meter.
- Asking patients about the use of nonprescription medicines like vitamin, herbal, or nutritional supplements.
- Encouraging patients to keep a list of medicines they are currently using.
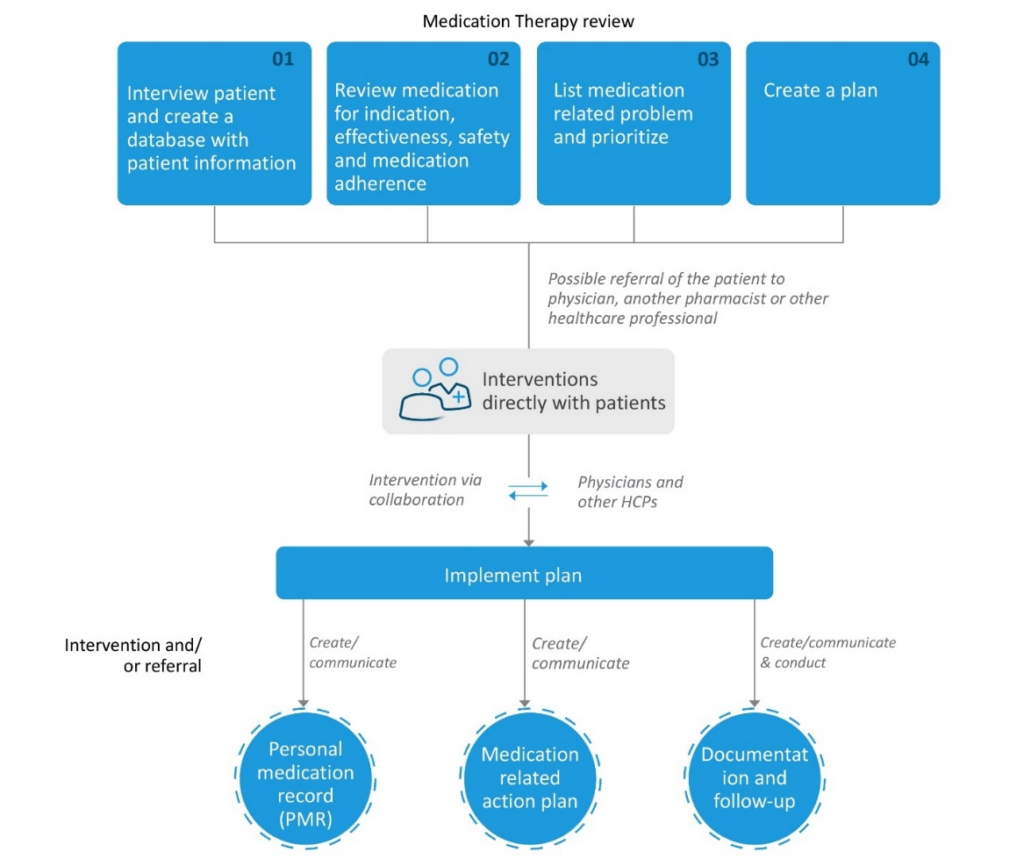
Figure 2: Flow Chart of a Medication Therapy Management Service Model. (This figure was created for illustrative purposes and is based on data obtained from American Pharmacist Association and National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model) 19.
Involvement of insurers:
Health insurance coverage is a first step toward access to care, disease management, and prevention of complications and comorbidities20. Insurers play a significant role in medication management by providing coverage for essential diabetes medications and supplies21. Here are several strategies insurers implement to ensure effective and efficient care of patients:
- Formulary management: Insurance providers typically maintain a formulary, which is a list of drugs covered under their plans. Diabetes medications, including insulin, are typically part of this formulary, and they may be categorized into different tiers that impact cost-sharing requirements for policyholders21.
- Pharmacy-benefit managers (PBM): PBM are third-party administrators that manage prescription drug benefits on behalf of health insurers. They negotiate with drug manufacturers for better pricing, manage formularies and process prescription drug claims22.
- Promoting medication adherence: Diabetes Self-Management Education and Support (DSMES) can provide evidence based knowledge to improve knowledge and skills to manage diabetes23.
Real-life examples of Medication management models:
ARMIN [Arzneimittel initiative Sachsen-Thüringen], the model of Saxony-Thuringia, was initiated in 2014 in Germany as a pilot project, for the establishment of better interprofessional medication management between general practitioners and community24. It was launched at the regional level, to increase medication safety among home-dwelling patients with polypharmacy, e.g., by reducing drug-related problems (DRPs) as well as increasing adherence24.
Conclusion:
Interprofessional medication management involving GPs, pharmacists, and insurers is essential for promoting diabetic adherence and improving patient outcomes. By working together, these stakeholders can address barriers to adherence, optimize therapy regimens, and empower patients to take control of their health. It is important that physicians and pharmacists have good communication because it is essential to go beyond transactional interactions to ensure optimal therapeutic outcomes for patients. Proper establishment of MTM is important to achieve the target. The value of MTM in clinical, economic, and humanistic terms is real and the results are both remarkable and replicable. Collaboration is the key to success in managing diabetes and reducing the burden of this chronic condition on individuals and healthcare systems alike.
“One thing that you really have to do is move forward. You’ve gotta really tackle this. You can’t be a passive patient.”
– Dr. Phil McGraw, an American television personality and author













