Rethinking pain adherence: From illness perception to behavioral solutions
- Pain is a sensory and an emotional experience resulting from a dynamic interplay of biological, psychological, and social factors and therefore is highly subjective in nature.1,2
- Adherence to pain medications is poor. The major barriers to adherence include dosing frequency, polypharmacy, pain intensity, and negative concerns about pain medications.3,4
- Approaches based on behavioral science, such as cognitive behavioral therapy (CBT), are an effective strategy to modify perception and behavior.5
Pain is a universal and primal sensation. It is among the most common reasons for primary care visits. As per the estimates, 1 in 5 patients complain of pain during their healthcare visit, either as the primary reason or due to an underlying cause.6,7
Pain is defined by the International Association for the Study of Pain as “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.” 2 The pain can be acute, may come and go, or it could be far more debilitating, persisting for months or even years.8 About 1 in 10 patients experience chronic pain every year,7 and according to some studies, its worldwide prevalence could be as high as 30%. Pain, especially the chronic ones, is debilitating, with a negative impact on daily activities, and is the leading cause of years lost to disability.1
Psychology of pain – It’s all about perception
Pain is classified into three types: acute, a short-term pain; intermittent, a condition where pain comes and goes; and chronic, which is a persistent, long-term pain.8 According to the biopsychosocial model of pain, the physical symptoms of pain result from a dynamic interplay of biological, psychological, and social factors.1
It is now well established that the pain experienced by a person is subjective.1,8 It varies from one person to another, with factors such as age, ethnicity, stress levels, and underlying disease further contributing to differences in perception.9 The brain plays a crucial role in perceiving and managing pain, and in many cases, it may not be directly correlated with the actual tissue damage. Although pain perception is influenced by the pain signals transmitted by the peripheral sensory systems, it is largely driven by the control mechanisms in the central nervous system, which modulate those signals and regulate pain perception. Therefore, educating patients about the processing of pain signals and pain perception by the brain’s pain centers is crucial for pain management.10
The biomedical treatment of pain is not uniformly effective among patients.10 As the pain perception varies, so does the perception of pain relief and response to the drug treatment.9 Therefore, the effect of pain medications on pain relief remains underwhelming, with some studies reporting an average efficacy of just 30% and on average, only 1 in 2-4 patients gets 50% relief from pain due to pharmacological treatment.4 Factors that contribute to variation in pain perception also influence the perception of pain relief. In addition, the pharmacogenetic variations further add to the differences in the perception of drug response and pain relief.9
Pain management – a multimodal approach
The current clinical paradigm for chronic pain management uses an interdisciplinary multipronged approach that encompasses pharmacotherapy, restorative, interventional, behavioral, complementary, and integrative health approaches.1,11 However, pain treatment remains challenging due to poor outcomes. Even with the use of complex multimodal approaches, the pharmacological interventions remain the cornerstone of pain management, which includes non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, antidepressants, opioids, and gabapentinoids.4,11
Non-adherence to pain medications is prevalent
Non-adherence to chronic pain medication is very high, with both underuse and overuse being common. As many as 30% patients are reported to use less medication than prescribed, while 14% overuse it.4 Suboptimal use of medications is known to lower the expected outcomes. On the contrary, overusing pain medications can have serious health consequences. Abuse or overdose of prescription opioids is known as the cause of thousands of fatalities. Therefore, non-optimal use of pain medication is a serious challenge. However, addiction and overuse of opioids are considered a separate issue from non-adherence, with different risk factors and management strategies.4
Determinants of non-adherence to pain medications
The factors affecting adherence to pain medications include dosing frequency, polypharmacy, low intensity pain, younger age, concerns about medication and poor patient-provider relationship, concerns about side effects, and addiction:
- Patient’s illness perception: Perception of illness is positively associated with adherence. Patient perceiving their condition as chronic, uncontrolled, and unremitting was found to be adherent. A perceived need was associated with overuse, while a less perceived need was associated with underuse. On the other hand, patients using other coping strategies and using self-medication were most likely to be non-adherent.4
- Health literacy: Education level, which can impact patients’ health literacy, was found to be an important factor associated with lower medication adherence. While knowledge of the prescribed pain medication was associated with higher adherence, lack of sufficient information about medication was cause of non-adherence.4
- Patient-provider relationship: Poor patient-provider relationship, mistrust, miscommunication, as well as patient satisfaction, were negatively associated with adherence.4
- Pain intensity: The Intensity of pain perceived is an important factor impacting medication adherence. Low-intensity pain was often reported to be associated with lower adherence rates, possibly due to a lower necessity perception.3,4
- Polypharmacy and dosing frequency: Both polypharmacy and high dosing frequency are reported to be negatively associated with medication adherence.4 Treatment complexity is a known factor to influence adherence to treatment; therefore, keeping the treatment regimen simple with the use of long-acting medicine is crucial.3
- Medication concerns: Attitude and concerns regarding the medication are an important determinant of non-adherence. Patients concerned about addiction, tolerance, side effects, and withdrawal symptoms were found to be less adherent.4
How can clinicians predict non-adherence to pain medication in practice?
It is essential to predict and identify non-adherence to pain medication in the general practice, and efforts have been made to stratify patients into risk categories, especially for opioid prescription. Multiple questionnaires can be used to assess and predict suboptimal adherence to pain medications, especially opioid prescriptions such as:
- Pain Medication Questionnaire (PMQ),
- Prescription Drug Use Questionnaire (PDUQ), and
- Diagnosis Intractability Risk and Efficacy Score (DIRE score)
Additionally, identifying associated risk factors such as polypharmacy, attitudes, and concern towards pain medications can help predict non-adherence in patients and provide scope for targeted interventions for such patients.12
Adherence to pain medications – beliefs and perceptions matter
Non-adherence can be “unintentional”, when a patient forgets to take medicine, fill a prescription, misunderstand the prescription, etc., or it can be “intentional”, a conscious decision based on the perceived necessity and concerns for the medication. Belief and perception towards pain medications are reported as the most significant issue in non-adherence.4,9,13 To explore more about how beliefs and perceptions influence medication adherence, please read our article Impact of belief and misconception in medication non-adherence
Unlike chronic asymptomatic conditions, where unintentional causes of non-adherence are dominant, in chronic pain, a symptomatic condition, it’s largely the intentional causes.4
A clinical study, examining the determinants of medication non-adherence in chronic pain, identified patient perception as the main cause of non-adherence to pain medications. Out of 13 causes identified, all but two were intentional related to patients’ necessity vs. concerns, beliefs, such as a perceived low necessity, concerns about side effects, and perceived non-efficacy. Therefore, it is essential to discuss and understand patients’ perspectives, particularly regarding their beliefs and concerns, and tailor the treatment course accordingly to minimize intentional non-adherence.13
Psychosocial therapy for changing behavior in pain management
Psychosocial methods for behavior change are often used as an effective approach in pain management, in addition to the routine biomedical and rehabilitation interventions. Cognitive behavioral therapy (CBT) is widely used to manage chronic pain in addition to the biomedical treatment. It promotes self-management techniques and self-control using structured tools to modify behavior and cognition.5
CBT is usually delivered individually or in group sessions over several weeks and is known to reduce pain perception by improving a person’s ability to cope with pain. It includes:14
- Cognitive restructuring – Identifying and managing negative thoughts and behaviors, and developing more adaptive coping strategies
- Relaxation techniques – Such as deep breathing and muscle relaxation methods, visualizing a reduction in muscle tension to alter pain perception
- Time- or quota-based activity pacing: A behavior strategy that involves scheduling activities based on time or quota despite persistent pain to maximize functionality
- Sleep Hygiene – refers to scheduling sleep timings and modifying diet, environment, or activities to maintain sleep quality and duration.
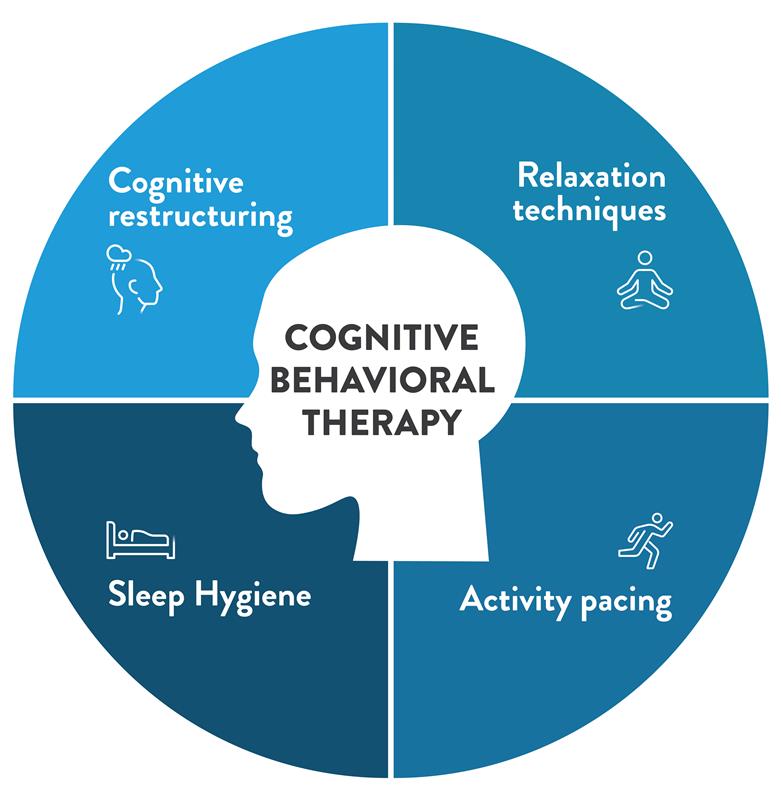
Figure 1: Components of Cognitive Behavioral Therapy (CBT) for chronic pain14
(The image is only for illustration purposes based on content from Knoerl et al., 201514 )
Effectiveness of CBT in pain management
Several studies have reported on the efficacy of CBT in chronic pain management. It reduces pain intensity, disability, distress, and healthcare use.5 Preliminary studies using Magnetic Resonance Imaging (MRI) have revealed CBT-induced changes in the prefrontal cortex that may lead to the production of pain-inhibiting neurotransmitters with the potential of decreasing the perception of pain. In a Cochrane review of randomized controlled trials, use of CBT as compared to standard care for pain management reported a beneficial effect on disability, mood, and catastrophizing of pain.14
Patients may sometimes feel overwhelmed by the complexity of CBT techniques. Therefore, studies have reported using fewer components of CBT techniques, such as relaxation or coping strategies, in combination with Motivational Interviewing (MI) in chronic pain management.5 Alternatively, interventions based on other theoretical psychological models, such as the Behavior Change Wheel based on Capability, Opportunity, Motivation (COM-B) model, have been applied to improve adherence to pain medications.15
Conclusion
Patients’ perception of the pain and pain relief in association with attitudes towards medication and concern about side effects are associated with non-adherence and outcome parameters.9 Behavioral theory-based interventions, such as CBT, MI, and COM-B, can help in improving medication adherence and therapy outcomes.5,15
According to the biopsychosocial model of pain, the physical symptoms of pain result from a dynamic interplay of biological, psychological, and social factors.1 The brain plays a crucial role in perceiving and managing pain, with factors such as age, ethnicity, stress levels, and underlying disease contributing to differences in pain perception. Therefore, biomedical treatment of pain is not uniformly effective among patients.9 As the pain perception varies, so does the perception of pain relief and response to the drug treatment. Therefore, the effect of pain medications on pain relief remains underwhelming, with some studies reporting an average efficacy of just 30%. All these factors impact adherence to pain medications.4
It is essential to discuss and understand patients’ perspectives, particularly regarding their beliefs and concerns, and tailor the treatment course accordingly to minimize intentional non-adherence due to fears of addiction. Interventions that enhance patients’ education and modify their beliefs and attitudes towards pain medication are important to alleviate their fears and change their behavior. Behavioral interventions like Cognitive Behavioral Therapy (CBT) and Motivational Interviewing can help to change the patient’s beliefs towards pain medication, leading to enhanced participation and adherence in chronic pain management.5
It is important to be able to predict and identify non-adherence to pain medication in clinical practice. Questionnaires such as PMQ, PDUQ, and DIRE scores can be used to assess and predict suboptimal adherence to pain medications. Identifying associated risk factors, such as polypharmacy, attitudes, and concern towards pain medications, can help predict non-adherence in patients and provide scope for targeted interventions for such patients.12
Perception towards pain medications is reported as the most significant issue in non-adherence.4 Clinical studies using CBT in chronic pain management report reduction in pain intensity, disability, distress, and healthcare use.5 Some preliminary studies also revealed CBT-induced changes in the brain that may lead to the production of pain-inhibiting neurotransmitters, potentially decreasing the pain perception. In a Cochrane review of randomized controlled trials, use of CBT as compared to standard care for pain management reported a beneficial effect on disability, mood, and catastrophizing of pain.14
Cognitive behavioral therapy (CBT) is widely used to manage chronic pain in addition to the biomedical treatment. They help patients to adapt to chronic pain by promoting self-management techniques and coping strategies using structured tools to modify behavior and cognition.5,14 This includes methods like identifying and managing negative thoughts, teaching relaxation techniques, scheduling activities to maximize functionality and maintaining sleep quality and duration.14













