Rx for change: Addressing social determinants to improve medication adherence
- Social determinants of health (SDH) encompass non-medical factors that influence health outcomes.1
- SDH is increasingly recognized as a significant predictor of medication non-adherence and healthcare engagement.2,3
- Interventions such as “social prescribing”, which address patients’ social needs, can bridge healthcare gaps and improve medication adherence.3,4
It is said that your “zip code” is a better predictor of health than your genetic code. Where you live often reflects your economic status, availability of jobs, education and training opportunities, as well as your access to healthy food, opportunities to exercise, and healthcare services.5 Medical care is estimated to account for only 10-20% of the modifiable factors that affect health outcomes. In contrast, the majority—80-90%—is influenced by social determinants of health (SDH).6
Inequities in power, money, and resources breed inequities in daily living conditions, leading to huge inequities in health.7 The importance of addressing these adverse social conditions to improve human health is aptly summarized by Professor Michael Marmot, a leading advocate for health equity, who states, “What good is it to treat people and then send them back to the same conditions that made them sick?”.7,8
The health gap: Role of social determinants
The World Health Organization (WHO) defines SDH as any non-medical factor influencing health outcomes. These relate to the person’s place of birth, the circumstances they grew up in, their age, and what they do for a living. It also includes all the other aspects that shape the conditions of their daily life like social and economic policies as well as political system.1 Social and living circumstances negatively impact health by contributing to a higher prevalence of chronic diseases and people’s ability to manage them.2 They are considered to be more important in influencing health than healthcare access and lifestyle choices. It is crucial to address these social barriers to improve health and achieve health equity.1
The impact of SDH can be observed through geographic disparities in human life expectancy, which serves as a crude metric of complex health outcomes.9 Life expectancy ranges from just 52 years in Sierra Leone and the Central African Republic to as high as 85 years in Japan and Hong Kong—a staggering difference of three decades. This variation is partly due to socioeconomic differences.10 Disparities in life expectancy are not only evident between countries but also within communities in the same nation, particularly between those at opposite ends of the socioeconomic spectrum.7,9 This underscores the significant impact of SDH, which are estimated to account for approximately 30–55% of health outcomes.1 Consequently, both the WHO and international treatment guidelines advocate for the assessment of SDH to enhance health outcomes.1,3,11
The key social determinants of health:12
- Economic stability: One of the most important determinants of health and health outcomes. Economic hardships due to poverty, job instability, or other factors can impact access to nutritional food, secure housing, and quality healthcare resulting in poor quality of life and health as well as deprioritizing management of health conditions.
- Education access and quality: Quality education prepares a person to navigate various life challenges. People with better education are more likely to live long and healthier lives as it ensures better job opportunities and relative economic stability. However, socioeconomic conditions often become a barrier to quality education.
- Healthcare access and quality: Access to quality healthcare is pivotal for managing chronic health conditions. Factors like geographic distance, cultural differences, and healthcare insurance can hinder access to quality healthcare.
- Neighborhood and built environment: The environment where we live and work has a bearing on health. Cleanliness in the neighborhood, air quality, access to green spaces, and community health impact an individual’s well-being.
- Social and community context: Social support and community networks play a pivotal role in an individual’s health. Social support is known to bring resilience, lower stress levels, and positive effects on well-being. Conversely, a lack of social and community support can bring adverse health outcomes.
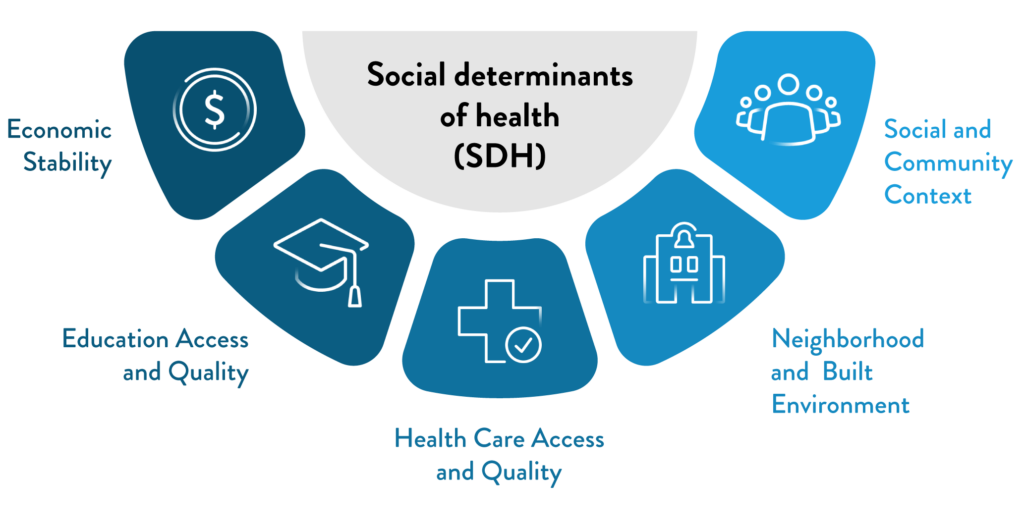
Figure 1: Social determinants of health
(The figure is for illustration purposes only. Adapted from Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.)12
Social determinants of health and medication adherence
SDH impacts health outcomes by influencing medication adherence.2 SDH is increasingly recognized as a strong predictor of access to and engagement with healthcare as well as health outcomes.13 Studies have shown that competing demands and life chaos negatively impact treatment adherence, while addressing unmet social needs can lead to improvements in adherence.14
Numerous studies have highlighted the impact of SDH on medication adherence among patients with chronic health conditions such as hypertension, diabetes, and HIV/AIDS.2,11,15,16 Both primary and secondary non-adherence to anticoagulants were reported to be significantly influenced by SDH factors such as race, insurance coverage, and employment status.16 A recent meta-analysis of these studies revealed a significant association between SDH and medication non-adherence. Specifically, housing instability and food insecurity were found to correlate strongly with poor adherence, indicating that patients often prioritize their basic needs over managing their health.2 Interventions aimed at improving medication adherence that do not take SDH into account have shown limited success in enhancing patient outcomes.3
The Z-codes: Standardizing SDH data documentation
To effectively use SDH for risk prediction, enhancing patient care, and facilitating data exchange between social services and healthcare providers, it is essential to capture SDH indicators within electronic health records. However, achieving a consistent and uniform collection of SDH data has proven challenging due to the lack of standardized screening tools and insufficient knowledge among providers.13,17
The “Z-codes,” which are part of the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), represent a set of codes designed to capture standardized SDH information.17 There are nine broad categories of Z-codes, each containing several sub-codes that allow for detailed documentation of patient information and risk stratification. These codes can be utilized in any healthcare setting and can support referrals to community and social services.13 Recent studies have begun to examine correlations between Z-scores and healthcare service utilization to assess potential clinical and financial implications.17
Addressing SDH through social prescribing
To effectively address SDH, it is important to implement non-medical interventions that can improve health behaviors. Social prescribing is one such novel intervention that is now gaining traction. This approach targets the social factors contributing to health issues, similar to how traditional prescribing targets the biological aspects of health problems.4
Social prescribing empowers general practitioners with tools to link clinical practice with social activities within the community. Physicians can refer patients to social prescribers also known as community connectors or link workers who evaluate a patient’s unique social circumstances and provide personalized referrals to target support groups and social or community activities for varying frequency and intensity depending on the individual’s requirement.3,4 A model of social prescription based on WHO toolkit for social prescribing is shown in Figure 2.
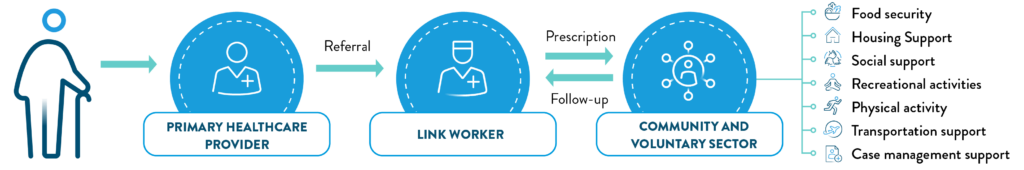
Figure 2: A pathway for social prescribing.
(The figure is for illustration purposes only and is adapted from WHO toolkit on how to implement social prescribing)18
Social prescribing in practice: Tips for general practitioners4
- Engage with voluntary community organizations and patient participation groups. Discuss with other local practices to identify a local lead to support social prescribing activities
- Focus on high-risk patients, such as those with chronic conditions, and incorporate social prescribing options into their annual care plans
- Educate patients about available social prescribing programs, and encourage them to take up the offer
- Develop a referral form that collects basic patient data and patient consent to share information
- Collaborate with link workers to define the referral criteria and feedback mechanisms
- Establish a system to collect patient feedback on social prescribing services, and prepare a plan to evaluate these services
Addressing SDH through pharmacist-led medication management services
Diabetes is one of the most common chronic conditions and adherence to diabetes treatment is known to be suboptimal. A recent study explored the role of SDH in adherence to diabetes treatment in older adults. The study showed the ability to afford balanced meals significantly impacted adherence.11
In a real-world study, the comprehensive medication management (CMM) telepharmacy service was expanded to include SDH support for diabetic patients from a disadvantaged background. The service included a comprehensive assessment to evaluate SDH in patients followed by pharmacist-led telehealth intervention to address them. The commonly raised SDH-related concerns were related to employment/income, medication access, transportation, health literacy and insurance status. These were addressed using interventions such as information provision/education, facilitating access to community resources, and coordinating additional patient care needs. The expanded services were rated as beneficial and highly satisfactory by patients increasing their SDH-self efficacy and quality of life.19
Communication is the key in addressing SDH to enhance adherence
Failing to identify patients’ hidden social challenges can lead to misdiagnosis and initiation of inappropriate care plans, exacerbating non-adherence to treatment. A survey on patients’ perception of services addressing social determinants found that over 40% of patients believed their primary care providers were unaware of their social struggles. To address this gap, clinical guidelines recommend a ‘selective inquiry’ approach, seamlessly integrating social history questions into patient encounters.20 Using brief targeted phrases about patients’ social needs during the medical interviews and improving coordination among healthcare teams can help effectively address SDH challenges in clinical practice.21
Patient-centered communication is crucial to address SDH and improving quality of care. Building trust with patients encourages open discussions about social and health-related needs. However, providers often struggle with time constraints and the lack of standardized tools to integrate SDH into electronic health records.21 a:care Insight is a validated predictive behavioral tool that helps providers identify patients at risk of non-adherence and the underlying factors contributing to it, including SDH. In addition, it provides personalized feedback to help forge the way forward to achieve better health outcomes.22













