Suspecting non-adherent behavior doesn’t hurt, overestimating it does!
- HCPs are key to identifying non-adherence, however, they often overestimate it in their patients
- The underlying reason for misjudging medication adherence in patients is thought to be HCP’s “optimistic bias”.
- Overestimating hinders early diagnosis of non-adherence and administration of the appropriate interventions1
A profoundly impactful statement by WHO captures the importance of medication non-adherence succinctly – “Increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatments”2. This effective intervention for improving patient health does not depend on any costly cutting-edge technology but a simple adherence to therapy which may not be a simple process by itself.
Adherence is an interplay between patient-related, HCP-related, and system-related factors. In one of our previous articles, we outlined the role HCPs can play in enhancing medication adherence in patients (HCPs role in adherence). They are best positioned to identify non-adherence in the initial stages and guide them toward more adherent behavior by providing suitable information and interventions. We also suggested that HCPs should work proactively to minimize non-adherence in their patient cohort. However, the problem comes when they fail to acknowledge that the problem exists.
Factors guiding HCP behavior and belief are less well-understood
Largely, patients’ beliefs have been researched and models built to understand what guides their behavior, but we do not understand what guides HCPs’ behavior and inherent biases. Various factors can influence the behavior of healthcare professionals which in turn can affect their clinical practice, such as3:
- Motivational predisposition to change
- Economic context
- Political beliefs
- Organizational conditioning
HCPs routinely overestimate adherence across several therapeutic areas
Non-adherence is a behavior that is crystalized by multiple factors. Estimation of non-adherence is a challenging task and there are various ways of estimating adherence (refer to our article on measuring non-adherence). It is well known that the most common method of adherence estimation – patient self-reporting – is prone to overestimation. However, not many HCPs appreciate the fact that their prediction or estimation of patients’ adherence behavior is also error-prone.
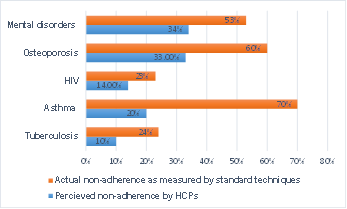
Several studies have consistently shown that HCPs, even ones with higher expertise or years of experience, overestimate non-adherence in the patients they treat. A study comparing the accuracy of non-adherence prediction in patients administering tuberculosis medications revealed a significant overestimation of adherence even by experienced HCPs (11%) as compared to the non-adherence assessed by laboratory-based methods (24%)4. Another study in asthma patients reported similar oversights in HCP’s estimation of medication non-adherence. Most of the study participants who were experts in lung diseases believed that only 10-20% of patients are non-adherent in the first 12 months of therapy initiation as opposed to published data that points to 60-80% non-adherence in this population. Ironically, two-thirds of the HCPs from this study were very sure of their estimates of non-adherence in the majority of cases, highlighting their error in judgments5. Similarly, for patients undergoing combined anti-retroviral therapy, HCPs overestimated adherence by 8.9% (86.2% vs. 77.3%)6. An osteoporosis study reported a similar pattern. Adherence estimates by HCPs were 67.2%, while the adherence assessed by the medication-possession ratio was only about 40%7. Along similar lines, the majority of HCPs (60%), although highly experienced in the field of mental health overestimated adherence in patients even after long-term association (>1 year) with them8.
All these studies highlight the discordance between the perception of HCPs about adherence and the actual adherence measured by any standard methods in their patients, even upon successfully establishing the HCP-patient relationship8. Please see Figure 1, which reports the mismatch in actual adherence as measured by standard methods and HCPs’ general perception of adherence in their patients, across treatment groups.
The reason for overestimating adherence – the “Optimistic Bias”
What is optimistic bias? As the name suggests it is a cognitive trait that influences our decision-making. While predicting the future, humans display an overwhelmingly positive attitude and routinely underestimate any negative possibilities. We are very optimistic about our future events and undervalue the chances of accidents, adverse events, or diseases. Therefore “optimistic bias” is defined as the difference between our perceptions or expectations vs. the actual reality or the outcome of a given scenario9.
Optimistic bias is a common and robust human trait that remains consistent even in the face of lifelong experiences with the reality that is often far from our expectations. Studies suggest that it is maintained throughout life as our beliefs are selectively influenced by our positive experiences and not by negative ones. It is well known that even experts are not immune to this bias and often make decisions influenced by it9. A recent landmark study on optimism bias among European physicians regarding anticipation of adherence behavior, specifically in their patients, reported a significant overestimation of therapy initiation and persistence. Importantly, the same HCPs were not so optimistic about medication adherence in other patients, highlighting the existence of a selective bias only for their patients1.
What causes the “Optimistic Bias” among HCPs for their patients?
Even though the presence of optimistic bias regarding one’s future is a known fact, what is not well understood is its influence on HCPs’ decision-making process for their patients. Besides medication non-adherence, the optimistic bias has been shown to affect HCPs’ perception of treatment outcomes and the survival of terminally ill patients10. Some possible causes suggested in the literature are:
- Self-serving bias: Motivation for perceiving one’s patient as better than others could emanate from a self-serving bias that serves a self-protective function. This results in perceiving these patients as an extension of themselves and matrics of their professional competence.
- Selective judgment: HCPs’ estimate of their patient’s adherence could be based on selective surveying. They could be affirming their adherence beliefs by cherry-picking information. They could be seeking out information from only those patients where they were confident of finding positive responses and ignoring the non-adherent pool.
- Superiority bias: Perception of superiority in themselves and over-confidence in the local health services may lead them to believe that their patients are better supported and therefore more adherent unlike others1.
- Contagion of optimism: Clinicians frequently overestimate treatment outcomes in patients displaying higher optimism bias. This is referred to as “emotional contagion”, a psychological state where one person’s optimism subconsciously rubs off on another person, in this case from patient to physician10.
Costs of overestimating adherence
We can eradicate any issue only if we acknowledge its existence. Unlike clinical trials, adherence in routine practice commonly relies on the judgment of patients or HCPs. In our earlier article, we highlighted the role of HCPs in identifying and preventing non-adherence as well as enhancing adherence to the prescribed treatment. On the contrary, as noted above, research has highlighted the oversight on HCPs’ part in underestimating non-adherence in their patients. This impacts,
- The identification of non-adherent behavior for moderately non-adherent patients.
- The uptake of preventive health behavior that could stem non-adherence in the early stages.
- Administration of appropriate interventions aimed at enhancing adherence5.
- Unnecessary changes in medications or dosage for patients showing poor treatment outcomes8.
Conclusions
Medication non-adherence is primarily driven by patients’ behavior, however many factors influence its manifestation. Healthcare professionals are at the forefront of identifying non-adherence and advise remedial measures to improve adherence. Therefore it is pivotal for HCPs to acknowledge the existence of this menace in their patients and be cautious of the influence of their own “optimistic bias” in their decision-making. Further, theory-driven research, similar to the ones that helped us to understand patient behavior, is required to discern HCP’s behavior and its driving factors to enable the formulation of appropriate interventions1.
“Doubt is often better than overconfidence because it leads to investigation and investigation leads to invention”
– Hudson Maxim












