Behavioral interventions to enhance adherence in oncology
- Adherence determines outcomes: Cancer therapies are only effective when patients take them as prescribed. For example, in chronic lymphocytic leukemia (CLL), missing ≥8 days of therapy in a phase 3 trial significantly shortened progression-free survival and doubled the risk of hospital admissions.6,7
- Behavioral science provides tools: Behavior models like the health belief model, social learning theory, behavior change technique taxonomy, and theory of planned behavior explain why patients may not adhere. They focus on beliefs, confidence, support, and control. These frameworks guide the design of effective adherence interventions in oncology.13–16
- Clinician involvement an essential pillar: Patients tend to have trust on their healthcare providers more than written materials. Meaningful interactions including regular follow-up, transparent communication, and proactive side effect management enhance adherence. Techniques rooted in behavior science like motivational interviewing and problem-solving can further enhance persistence with therapy.14
- Interventions must be tailored: Education alone rarely improves adherence in cancer care. Instead, multi-faceted approached i.e. utilizing digital tools, reminders, counseling, and psychological support are far more effective. Tailoring these interventions to the individual’s age, symptoms, and psychological state is crucial for achieving better outcomes.2,6, 10, 11,16–18
Cancer is a complex and life-threatening disease.1,2 It is often diagnosed at an advanced stage which results in high mortality.2 The high severity of the disease and the possibility of rapid progression demand early detection and timely approach to treatment.3 Delaying initiating therapy can have profound impacts on survival.4 Recent technological advances have resulted in therapies capable of slowing disease progression, extending life or achieving remission.2,4 Nonetheless, adherence to treatment remains the cornerstone for the effectiveness of cancer therapies.2,5
The importance of medication adherence in oncology
Non-adherence undermines therapeutic outcomes, increases risk for disease progression, mortality, poor quality of life and increased economic burden.6 The phase-3 RESONATE trial clearly demonstrated these consequences in patients with chronic lymphocytic leukemia. Patient who missed ≥8 consecutive days of treatment had a shorter median progression-free survival compared to patients who missed <8 days (10.9 months vs. not reached). Additionally, nonadherence resulted in two-fold increase in preventable, medication-related hospital admissions.7
In such scenarios, behavioral science provides frameworks to address adherence, considering patient, therapy, disease, and healthcare system factors.2
Behavioral science: A framework for understanding adherence
Behavioral science involves the study of human behavior through psychology, sociology, and economics.8 Moreover, it also contributes to clarifying the design of interventions intended to promote healthier behavior.
In oncology, behavioral science can help identifying barriers to adherence, understand patient decision-making and develop tailored interventions.2,6,9
Identifying risks to medication adherence in cancer therapy
Medication adherence is a complex issue, with a range of obstacles that must be understood in order to make meaningful improvements. These barriers can be due to patient itself, clinician, treatment or broader socioeconomic factor. As illustrated in Figure 1, each of these elements can interfere with consistent medication use.
- Patient-related factors: Many patients face challenges related to limited health literacy and poor understanding of their disease. Patients may mistakenly believe that they are cured and abandon treatment prematurely. Others may struggle with trust in the benefits of therapy or simply forget to take their medication.2,6 Comorbid conditions and fatigue can further complicate adherence.2,7
- Treatment-related factor: Treatment-related factors play a key role in medication nonadherence. Side effects, complex dosing schedules, and drug interactions often make it difficult for patients to stay consistent.7,9 Side effects are a main cause why patients quit taking their cancer medications.7 If the side effects are not managed well, they can become annoying and lead patients to skip doses or stop treatment altogether.8 A large patient survey found that people who didn’t experience side effects were more likely to stick to their treatment. More importantly, patients who felt their side effects were managed showed better adherence than those who didn’t.10
When a regimen involves multiple doses per day, it can be overwhelming. A systematic review of 76 trials showed that adherence drops as dosing frequency increases. Patients taking medication four times a day had an average adherence rate of just 50%, with some as low as 31%.6 Even when drugs are not taken daily, remembering the schedule can be tricky. For instance, generally pan-deacetylase inhibitor must be taken three times a week, while proteasome inhibitor is taken once weekly. Immunomodulator used in multiple myeloma treatment follows a simpler daily schedule for two or three weeks, followed by a rest week. However, it’s often combined with steroids and other agents like proteasome inhibitor which adds complexity, especially for patients with cognitive challenges.7 - Healthcare provider-related factors: Poor communication between patients and healthcare providers can lead to nonadherence. When patients feel dissatisfied with their care, they may not follow treatment plans. Lack of proper follow-up or after-care is another issue. In many cases, patients struggle as they are not given enough information or education about their condition and treatment.2,7,9
- Socioeconomic factors: Socioeconomic difficulties are also important determinant of medication adherence. Patients from lower-income backgrounds experience financial pressure due to the high cost of cancer medication. Some patients have no insurance or inadequate coverage, leading with high out-of-pocket cost. This can force them to skip doses, split pills, or stop treatment completely. A study analyzing claims data from CML patients found that medications with higher costs were associated with lower adherence rates.7 Limited access to treatment clinics and medication adds to the problem. Many also lack support from family and caregivers.7,9
In recent times, responsibility for medication has shifted from healthcare facilities to patients administering treatments independently at home. While this development is more convenience, it undeniably brings a lot of challenges and concerns. One major disadvantage is the increased risk of patients not sticking to their treatment plans.11 Self-administered cancer treatments have reported rates of adherence ranging from 20% to 100%. Poor adherence is associated with worse health outcomes and higher healthcare costs.11 These figures show the seriousness of the problem and highlight the need for effective interventions to help patients take their medications as prescribed.
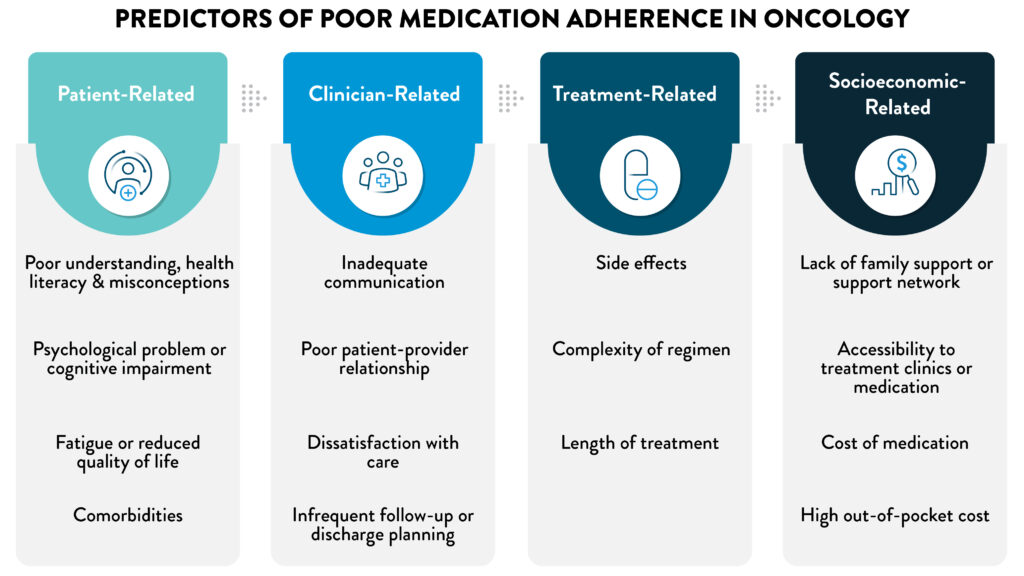
Figure 1: Factors contributing to medication nonadherence
(The image is only for illustration purposes and the content is from Reshma V. 2024, Cheung WY. 2013)2,9
Understanding adherence through behavioral science mode
Oral cancer therapies shift adherence responsibility to patients, increasing risk if not followed correctly.11-12 Behavioral science provides structured models to understand why patients fail to adhere and how behavioral interventions can improve outcomes.12
The few such frameworks of relevant to oncology are the health belief model, social learning theory with self-efficacy, behavior change technique taxonomy and theory of planned behavior:
- Health belief model (HBM): It suggests that people are more inclined to adopt a health behavior if they feel at risk and consider the action useful. Adherence improves when individuals regard their disease as serious, perceive themselves personally at risk, and are convinced that the benefits of treatment justify any drawbacks or cost. This model shows that whether willingness to change can shift with perceived risk or improvement upon the arrival of better treatments.13
- Social learning theory (SLT): SLT is a foundational model for understanding how behaviors are acquired and modified. It asserts that behavior is learned through various experiences, including observation and the consequences of actions. For example, taking a painkiller to relieve a headache reinforces that behavior if the outcome is positive. Immediate consequences tend to influence behavior more strongly than delayed ones. This explains the difficulty in sustaining health behaviors, especially when benefits are long-term or uncertain, and side effects are immediate. Adherence challenges often arise with medications for asymptomatic conditions like hypertension or those with adverse effects, such as neuroleptics.13
- Behavior change technique taxonomy (BCTT): This structured tool is suitable for designing and evaluating adherence interventions. Unlike the conceptual models above, BCTT is the standardized classification of 93 distinct behavior change techniques (BCTs). BTCs are classified into clusters such as goal setting, problem solving, feedback, and “social support.14,15
- Theory of planned behavior (TPB): TBP explains how people make decisions about engaging in intentional behaviors. In fact, the framework shows that a individual’s behavior is guided by their intentions, and those intentions are shaped by three key factors: their personal evaluation of the behavior, person’s beliefs about whether significant others think he/she should engage in the behavior, and their perceived capacity to have control concerning the behavior. These factors themselves are driven by beliefs about the potential outcomes, anticipated social reactions, and perceived obstacles. In this sense, behavioral intentions act as pivotal link between underlying beliefs and actual behavior.16
Integrating behavioral models in oncology care
- Swallowing exercises in head and neck cancer: This review discussed the influence of behavior change strategies concerning adherence to swallowing exercises in head and neck cancer. A systematic review of 15 trials revealed that 20 BCTs acted under three functional categories. Some studies showed no difference between groups, although they used the same type of BCTs. The BCTs that occurred more frequently in effective interventions, were practical social support, behavioral practice, self-monitoring of behavior and credible source for example a skilled clinician delivering the intervention. One trial showed that in a sham group using similar BCTs were better than those in a non-active control, pointing at the power of behavioral attention and action.15
- Hormonal therapy in breast cancer: A systematic review investigated five behavioral interventions for improving adherence to adjuvant hormonal therapy. All interventions included educational materials and reminders. However, none showed significant improvements in adherence in their primary analysis with 6014 patients (OR 1.03 to 2.06). The authors concluded that simply providing educational materials alone might not be sufficient. More personalized and comprehensive approaches are essential. A notable example was the COMPAS study, which implemented both motivational letters and phone calls based on by motivational interviewing techniques. While the primary analysis showed no significant difference, pooled data indicated that adherence was higher in the intervention groups compared to usual care.17
- Gamification (video-game intervention) with “Re-Mission” for young cancer patients: In a large, randomized trial across 34 centers in the United States, Canada, and Australia, 375 adolescents and young adults with cancer participated in a novel behavioral intervention. Patients were randomized to either a commercial video game or the same unit plus “Re-Mission”. A game focused on cancer where the players were controlling a nanobot that destroys cancer cells and managing treatment side effects. The intervention group had significantly higher adherence as confirmed by metabolite levels and electronic pill cap reading (16% greater adherence). Participants also perceived greater knowledge and self-efficacy, but self-reports of adherence, stress and quality of life scores remained unchanged.18
- Depression and planned behavior in post-radiation patients with breast cancer: One of the effect depression manifests in patient with breast cancer is decreased adherence to the treatment. This study shows that TPB explains how depression affects both intentions and actual use of medication. Data were collected from 213 women, revealed that depression was linked to poor attitudes and low perceived control, which weakened intentions and reduced adherence. Structural models confirmed that TPB fully mediated this relationship. Improving attitudes and boosting perceived control like helping with access to medication may support better adherence.16
- Healthcare profession interventions for oral cancer therapy adherence: A systematic review of healthcare professional implemented interventions involving 1,654 adult cancer patients on oral targeted therapy. All the studies concluded that healthcare professional-led interventions significantly improved adherence to oral targeted anticancer medicines. Clinicians support had much higher odds of continuing treatment (OR 17.91; 95% CI 3.18–100.73) and achieving adherence thresholds MPR ≥90% (OR 3.67; 95% CI 1.98–6.80) compared to usual care. Commonly used BCTs were “credible source,” “problem-solving,” “instruction on how to perform a behavior,” and “pharmacological support.”14
- Behavioral interventions for oral therapy adherence in breast cancer: This was the first systematic review to apply the BCTT to interventions directed at adherence to oral therapies in breast cancer. Thirty-six studies were reviewed involving 28,528 patients. Most interventions used eHealth tools, particularly mobile apps, while others were based on in-person visit or written materials. Common techniques included “problem solving,” “social support,” “information about health consequences,” and “prompts/cues.” Fifteen studies used the social cognitive theory and cognitive behavioral therapy in their theoretical frameworks. Other models included the health belief model, theory of planned behavior, and acceptance and commitment therapy.
Interventions varied in format i.e. apps, phone calls, videoconferencing, written materials. Five eHealth studies showed improved adherence, mostly through apps with reminders and tracking. In-person interventions led by nurses or psychologists also showed positive results. Written materials had mixed outcomes. Some studies tested unique approaches like blister packs, dietary changes, or personalized follow-up. Across all formats, 25 BCTs were identified. The most frequent were “problem solving,” “social support,” “information about health consequences,” and “prompts/cues.” Effective interventions often included “feedback on behavior” and tailored support.12 - Tailoring behavioral interventions for AET adherence in breast cancer: In an exploratory analysis of a parallel, randomized-controlled trial, the STRIDE intervention was delivered virtually in six weekly, hour-long group sessions led by a psychologist. Cognitive behavioral and motivational interviewing techniques were used for skills-based interventions, as needed including relaxation, cognitive reframing, acceptance, and side effect management. Age (B = 0.05, SE = 0.02, p = 0.003) and AET-related symptom distress (B = −0.04, SE = 0.02, p = 0.02) moderated the effect of STRIDE on self-reported adherence, however anxiety (B = −1.20, SE = 0.53, p = 0.03) and depressive symptoms (B = −1.65, SE = 0.65, p = 0.01) moderated objective adherence. Older patients and those with lower anxiety, depressive symptoms, or symptom distress showed greater adherence gains. These findings suggest that behavioral interventions like STRIDE may be most effective for patients with fewer psychological or physical symptoms.19
Therefore, applying behavioral science in oncology has moved beyond theory into practical interventions across varied settings. From breast cancer hormonal therapy to head and neck swallowing exercises, digital games for young patients, and structured clinician-led programs, such models highlight how tailored strategies can be used to address barriers.14,15,17,18 Improved adherence leads to better survival, enhanced quality of life, and reduced healthcare costs (Figure 2).
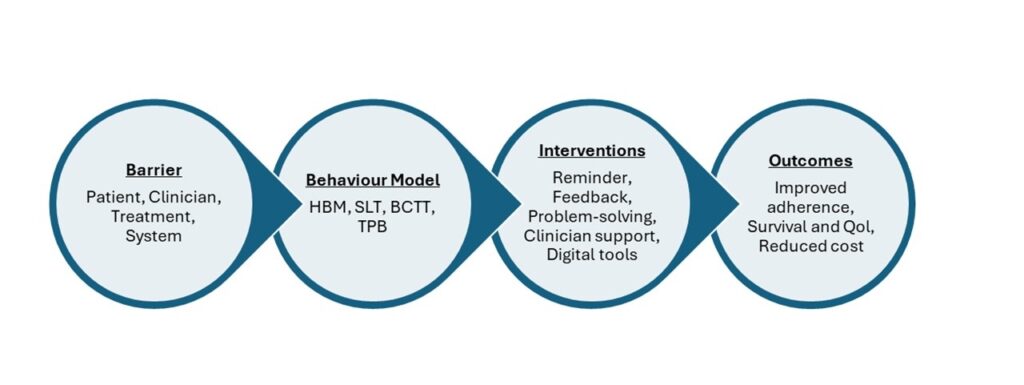
Figure 2: Behavioral science pathway to adherence in oncology
(The image is only for illustration purposes and the content is from Reshma V. 2024, Cheung WY. 2013, Kehoe WA 1998, Angus F 2025, Govender R 2017, Manning M 2011, Hurtado-de-Mendoza A2016 and Walsh EA 2024).2,8,12-16,18
Conclusion
Early detection and timely intervention are undeniably pivotal when it comes to cancer outcomes. While modern therapies can extend survival, their benefits rely on patient adherence. Nonadherence increases relapse risk and financial burden. Behavioral science helps address this challenge by identifying barriers and guiding tailored interventions. Approaches like the Health Belief Model, Social Learning Theory, Theory of Planned Behavior, and the BCT Taxonomy offer useful frameworks. Evidence shows that digital tools, psychoeducation initiatives, and patient-centered counseling can improve adherence. The next step is integrating these strategies into routine oncology care to ensure therapies lead to better survival and quality of life.
Answer: Because adherence to medication is critical for treatment outcomes. Even brief interruptions can accelerate disease progression. Data from the RESONATE trial support this and showed that missing over eight days of therapy leads to much shorter progression-free survival compared with those who adhered to more than 8 days.7 It’s just not survival, missing therapy means more hospital admissions and increased healthcare costs.11
Answer: Side effects are a leading driver of discontinuation.7 Patients frequently stop therapy if drug toxicities are not managed proactively. Complexity of regimens is another barrier. A systematic review shows adherence declines steeply as dosing frequency increases.7 For instance, adherence can drop to 50% or lower when four doses per day are required.7 Simplifying regimens and active side-effect management are key clinical strategies to overcome these challenges.
Answer: Financial toxicity is also a strong predictor of poor adherence.7 High out-of-pocket costs, lack of insurance, and limited access to pharmacies or treatment centers often force patients to skip doses or stop treatment altogether.7 Family or caregiver support also matters. Patients without reliable support networks often report lower adherence. Screening for financial and social barriers should be part of routine oncology care.7
Answer: Actually, clinician’s role is pivotal.2 Evidence clearly shows that the treating physician or nurse has a stronger impact on adherence.14 Patients value follow-up, reassurance, and clear instructions on how to take medicines.7 Communication is therefore both a therapeutic tool and a behavioral intervention.7 Structured follow-ups, motivational interviewing, and timely toxicity management enhance adherence significantly.7,17
Answer: Behavioral science gives a framework to figure out actual reasons why patients drop off. It combines insights from psychology, sociology, and economics.8 This helps us move beyond “patient forgot” explanations, allowing identification of underlying drivers such as beliefs, side-effect fears, or socioeconomic stressors.6 More importantly, it informs structured interventions that can be integrated into daily practice.
Answer: A few models have strong clinical relevance. The Health Belief Model looks at how risky patients think their condition is and whether they believe that the therapy would actually help.13 Social Learning Theory explains that behavior is learned through experience, observation, and consequences.13 The Theory of Planned Behavior focus on attitudes, social pressure, and perceived control.13 Finally, the Behavior Change Technique Taxonomy provides strategies like goal-setting, and action planning.15 Each model offers a lens to guide patient-centered interventions.
Answer: Digital tools like mobile apps, SMS reminders, and electronic pill caps can improve adherence, but rarely in isolation.7,8,12 They work better alongside human interactions such as nurse check-ins, clinician feedback, or motivational counseling.12,19 Studies in breast cancer therapy show that technology like eHealth interventions work best when integrated into a broader support system rather than as stand-alone reminders.12













